Annotated-final chloramphenicol PDF
| Title | Annotated-final chloramphenicol |
|---|---|
| Author | Simona Borriello |
| Course | From patient to gene |
| Institution | University of Sunderland |
| Pages | 5 |
| File Size | 168.5 KB |
| File Type | |
| Total Downloads | 96 |
| Total Views | 124 |
Summary
Pharmacokinetics, pharmacodynamics and mode of action of chloramphenicol ...
Description
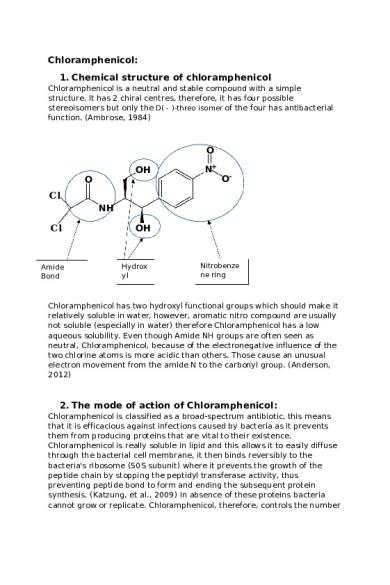
Chloramphenicol: 1. Chemical structure of chloramphenicol Chloramphenicol is a neutral and stable compound with a simple structure. It has 2 chiral centres, therefore, it has four possible stereoisomers but only the D( - )-threo isomer of the four has antibacterial function. (Ambrose, 1984)
O OH O
N+
O-
Cl NH Cl
Amide Bond
OH
Hydrox yl
Nitrobenze ne ring
Chloramphenicol has two hydroxyl functional groups which should make it relatively soluble in water, however, aromatic nitro compound are usually not soluble (especially in water) therefore Chloramphenicol has a low aqueous solubility. Even though Amide NH groups are often seen as neutral, Chloramphenicol, because of the electronegative influence of the two chlorine atoms is more acidic than others. Those cause an unusual electron movement from the amide N to the carbonyl group. (Anderson, 2012)
2. The mode of action of Chloramphenicol: Chloramphenicol is classified as a broad-spectrum antibiotic, this means that it is efficacious against infections caused by bacteria as it prevents them from producing proteins that are vital to their existence. Chloramphenicol is really soluble in lipid and this allows it to easily diffuse through the bacterial cell membrane, it then binds reversibly to the bacteria's ribosome (50S subunit) where it prevents the growth of the peptide chain by stopping the peptidyl transferase activity, thus preventing peptide bond to form and ending the subsequent protein synthesis. (Katzung, et al., 2009) In absence of these proteins bacteria cannot grow or replicate. Chloramphenicol, therefore, controls the number
of bacteria while the body's immune system kill the remaining ones. This eliminate the infection.
(Katzung, et al., 2009) Figure 1. In step 1, the charged tRNA carrying the amino acid 6 binds to the acceptor side on the 70s ribosome subunit. The amino acid chain (1 to 5) then binds to amino acid 6 in step 2. The uncharged tRNA is released in step three and the new tRNA along, with the new 6 amino acid chain shift to the peptidyl site (4). Chloramphenicol, shown as a C, binds to the 50s subunit and prevent step 2 from taking place.
3. The pharmacokinetics of Chloramphenicol: 3.1 Dose and absorption: The usual dosage of Chloramphenicol is 50-100 mg/kg/d; after oral assumption the crystalline chloramphenicol is quickly absorbed completely. A 1 g dose usually induce blood levels between 10 and 15 mcg/ml. It penetrate widely to all the tissues and body fluids, including the brain tissue. Chloramphenicol penetrates the cell membrane without difficulties. (Katzung, et al., 2009) 3.2 Half-life:
The half-life in adults with not alterated renal and hepatic functions is between 1.5 and 3.5 hours. However, in patients with damaged renal function the half-life is 3-4 hours. If the patient has severely damaged hepatic functions the half-life increase to 4.6 to 11.6 hours. In children from 1 month to 16 years old is between 3 and 6.5 hours while it dramatically increase in infants (1/2 days old) which is usually 24 hours but this is really variable. (Drug Bank , 2017)
3.3 Biotransformation and Elimination: The conjugation with glucuronic acid in the liver or the reduction of inactive aryl amines leads to the inactivation of most of the drug (about 90% of the total dose administered). Both, active and inactive chloramphenicol are eliminated in the urine. A small amount of the active part it is also excreted in the feces. (Katzung, et al., 2009) 3.4 Shelf life: Chloramphenicol has a shelf life of several years and it is able to retain 100% of its activity for 24 hours in a solution with a PH range of 1-9.5. However, if it is exposed to light for a long time it degrades in the solution. (Anderson, 2012)
4. How the drug is used in practice: 4.1 Clinical uses of Chloramphenicol: The spectrum activity of Chloramphenicol is really wide, it is in fact active against Gram positive and Gram negative bacteria. However, Because of its serious adverse effects, Chloramphenicol use it is been restricted to treating life-threatening infections such as Haemophilus influenza meningitis. Most commonly topical chloramphenicol is used for treatment of bacterial conjunctivitis mainly through eye drops or ointments. (Neal, 2016) Chloramphenicol, is also available as an ear drop preparation, it used to treat otitis externa which is an inflammation of the external ear canal. However, they are not really recommended as they contain propylene glycol which, in high concentration, could lead to hear damage. Another, but more uncommon use of this drug is to treat epiglottitis through intravenous Chloramphenicol. And occasionally it is used to treat Typhoid fever. (Anderson, 2012) 4.2 Side effects: Chloramphenicol may cause nausea, diarrhoea or vomiting, also vaginal or oral candida may occur because of the changes of the microbial flora. One of the most dangerous sides effects of Chloramphenicol is Aplastic anaemia, it usually occurs after prolonged use and it is often fatal and
irreversible. The danger of Aplastic Anaemia is sufficiently high that other options should be considered. The impact for the most part happens weeks or months after the treatment has been ended. Because of the lack of glucuronic acid conjugation mechanism (needed for the deactivation and detoxification of the drug) in infant, it may be toxic to them. Therefore, when an infant is administered with dosages above 50mg/kg/d, the drug may accumulate and lead to grey baby syndrome which includes vomiting, hypothermia, grey skin and sometimes collapse. (Katzung, et al., 2009) 4.3 Cautions and contraindications:
According to the BNF, when chloramphenicol is used intravenously or orally it could lead to acute porphyria. When used by ear avoiding a prolonged use is essential. With intravenous use or oral use it is also important to don't use it for a long time and to avoid repeated courses. (BMJ Group and the Royal Pharmaceutical Society of Great Britain , 2017) To avoid toxicity in infants, chloramphenicol should be used carefully with a dose limit of 50mg/kg/d or less, dose should be lower in premature infants (25mg/kg/d). (Katzung, et al., 2009) For the same reason, the use of oral or intravenous chloramphenicol should be avoided during pregnancy as it could lead to "grey baby syndrome" if used in the third semester. Topical chloramphenicol should also be avoided during pregnancy unless it is essential. The use of chloramphenicol should be avoided when breast feeding, even though the concentration in milk is not enough to lead to baby grey syndrome it may still cause bone marrow toxicity in new-borns. In patients with hepatic and renal impairment the use of chloramphenicol should be avoided, if possible, or the dose should be reduced as there is an increased risk of bone-marrow depression. Also, in patient with hepatic impairment plasma-chloramphenicol concentration should be monitored. (BMJ Group and the Royal Pharmaceutical Society of Great Britain , 2017)
References Ambrose, P. J., 1984. Clinical Pharmacokinetics of Chloramphenicol and Chloramphenicol Succinate. Clinical Pharmacokinetics, Issue 9, pp. 222-238. Anderson, R. J., 2012. Chloramphenicol. In: Antibacterial agents: chemistry, mode of action, mechanisms of resistance, and clinical applications. Oxford: WileyBlackwell, pp. 232-239. BMJ Group and the Royal Pharmaceutical Society of Great Britain , 2017. BNF. London : Pharmaceutical Press.
Drug Bank , 2017. Drug Bank. [Online] Available at: https://www.drugbank.ca/drugs/DB00446 [Accessed 30 October 2017]. Katzung, B. G., Masters, S. B. & Trevor, A. J., 2009. Chemoterapeutic drugs. In: Basic & clinical pharmacology. New york: McGraw-Hill Medical, p. 802. Katzung, B. G., Masters, S. B. & Trevor, A. J., 2009. Tetracycline, macrolides and others. In: S. B. M. A. J. T. Bertram G. Katzung, ed. Basic & clinical pharmacology. New yorok: McGraw-Hill Medical, pp. 797-803. Neal, M. J., 2016. Antibacterial drugs that inhibit protein synthesis: aminoglycosides, tetracyclines, macrolides and chloramphenicol. In: Medical pharmacology at a glance. s.l.:Wiley-Blackwell, p. 181....
Similar Free PDFs

Annotated-final chloramphenicol
- 5 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu