Brittany Long v SIM Care Plan PDF
| Title | Brittany Long v SIM Care Plan |
|---|---|
| Course | Nursing Care of the Childbearing Family |
| Institution | Raritan Valley Community College |
| Pages | 10 |
| File Size | 443.4 KB |
| File Type | |
| Total Downloads | 96 |
| Total Views | 140 |
Summary
Download Brittany Long v SIM Care Plan PDF
Description
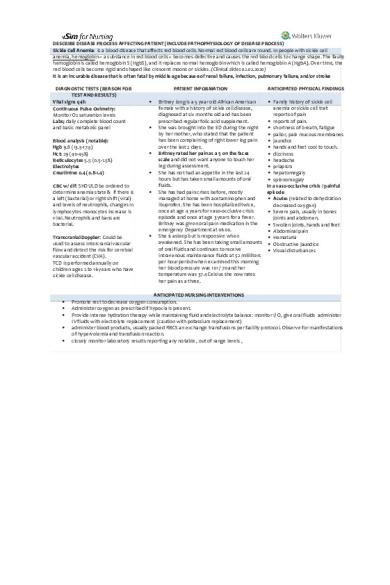
DESCRIBE DISEASE PROCESS AFFECTING PATIENT (INCLUDE PATHOPHYSIOLOGY OF DISEASE PROCESS) Sickle Cell Anemia: is a blood disease that affects red blood cells. Normal red blood cells are round. In people with sickle cell anemia, hemoglobin – a substance in red blood cells – becomes defective and causes the red blood cells to change shape. The faulty hemoglobin is called hemoglobin S (HgbS), and it replaces normal hemoglobin which is called hemoglobin A (HgbA). Over time, the red blood cells become rigid and shaped like crescent moons or sickles. (Clinical slides 02.02.2020) It is an incurable disease that is often fatal by middle age because of renal failure, infection, pulmonary failure, and/or stroke DIAGNOSTIC TESTS (REASON FOR TEST AND RESULTS) Vital signs q4h Continuous Pulse Oximetry: Monitor O2 saturation levels Labs; daily complete blood count and basic metabolic panel Blood analysis (notable): Hgb 9.8 (13.5-17.5) Hct: 29 (40-45%) Reticulocytes 5.5 (0.5-1.5%) Electrolytes Creatinine: 0.4 (0.8-1.4) CBC w/ dif: SHOULD be ordered to determine anemia state & if there is a left (bacterial) or right shift (viral) and levels of neutrophils, changes in lymphocytes monocytes increase is viral. Neutrophils and bans are bacterial. Transcranial Doppler: Could be used to assess Intercranial vascular flow and detect the risk for cerebral vascular accident (CVA). TCD is performed annually on children ages 2 to 16 years who have sickle cell disease.
PATIENT INFORMATION
ANTICIPATED PHYSICAL FINDINGS
Britney long is a 5 year old African American Family history of sickle cell female with a history of sickle cell disease, anemia or sickle cell trait diagnosed at six months old and has been reports of pain prescribed regular folic acid supplement. reports of pain. She was brought into the ED during the night shortness of breath, fatigue by her mother, who stated that the patient pallor, pale mucous membranes has been complaining of right lower leg pain jaundice over the last 2 days. hands and feet cool to touch. Britney rated her pain as a 5 on the faces dizziness scale and did not want anyone to touch her headache leg during assessment. priapism She has not had an appetite in the last 24 hepatomegaly hours but has taken small amounts of oral splenomegaly fluids. In a vaso-occlusive crisis / painful She has had pain crises before, mostly episode managed at home with acetaminophen and Acute: (related to dehydration ibuprofen. She has been hospitalized twice, decreased oxygen) once at age 4 years for vaso-occlusive crisis Severe pain, usually in bones episode and once at age 3 years for a fever. joints and abdomen. Britney was given oral pain medication in the Swollen joints, hands and feet emergency Department at 0600. Abdominal pain She is asleep but is responsive when Hematuria awakened. She has been taking small amounts Obstructive jaundice of oral fluids and continues to receive Visual disturbances intravenous maintenance fluids at 52 milliliters per hour period when examined this morning her blood pressure was 101 / 70 and her temperature was 37.4 Celsius she now rates her pain as a three.
ANTICIPATED NURSING INTERVENTIONS Promote rest to decrease oxygen consumption. Administer oxygen as prescribed if hypoxia is present. Provide intense hydration therapy while maintaining fluid and electrolyte balance: monitor I/ O, give oral fluids administer IV fluids with electrolyte replacement (caution with potassium replacement) administer blood products, usually packed RBCS an exchange transfusions per facility protocol. Observe for manifestations of hypervolemia and transfusion reaction. closely monitor laboratory results reporting any notable , out of range levels ,
vSim ISBAR ACTIVITY INTRODUCTION
STUDENT WORKSHEET This is Carly in the Pediatric Unit at the Our Lady Ginsburg Ruth Bader Hospital
Your name, position (RN), unit you are working on SITUATION Patient’s name, age, specific reason for visit
mg Patient’s primary diagnosis, date of admission, current orders for patient
ASSESSMENT Current pertinent assessment data using head to toe approach, pertinent diagnostics, vital signs
RECOMMENDATION Any orders or recommendations you may have for this patient
I am calling regarding Brittany Long, 16kg. Brought into the ED by her mother last night. Patient C/C right lower leg pain over the last 2 days. Rates pain at 5 on the FACES scale
Brittany Long was diagnosed with sickle cell disease at 6 months old. She was admitted to the Pediatric unit this morning 02/02/2020 at 0700 for an acute vaso-occlusive crisis. Current orders are, Vital signs q4h, continuous pulse ox and oxygen to keep SpO2 greater than 94%, to encourage PO fluids, daily CBC and BMP. D5 in 1/2NS IV at 52 mL per hour, codeine elixir 8 milligrams orally every four hours (06-10-14-18-22-02) , acetaminophen Alexa are 240 mg orally every six hours (6-12-18-24), ibuprofen elixir 160 mg orally at 0900 and then q6h , Docusate sodium 100 mg orally once daily at 2000, morphine sulfate 2 mg IV one time dose. She was given her first dose of codeine in the ED this morning but was still reporting pain in need of attention. Sigle prn dose of morphine 2mg was administered. ECG: normal Sinus rhythm. Heart rate: 126. Pulse: Present. Blood pressure taken at right upper arm via non-invasive BP cuff: 109/74 mmHg. Respiration: 24. Conscious state: Appropriate. SpO2: 99%. Temp: 37.3. The breath sounds are clear and equal bilaterally. regular heart sounds without murmurs. Pain reported at 3, assessed on the FACES scale. No known allergies, immunizations are up to date.
I recommend close monitoring of pain levels, strict I/Os to asses dehydration status with a possible increase in fluids needed.
PATIENT EDUCATION WORKSHEET NAME OF MEDICATION, CLASSIFICATION, AND INCLUDE PROTOTYPE
MEDICATION: Codeine elixir 8 mg PO q4h
CLASSIFICATION: THERAPEUTIC CLASS; cold and cough remedies, antitussives, opioid analgesics. PHARM CLASS; opioid agonists.
PROTOTYPE: Morphine
SAFE DOSE OR DOSE RANGE, SAFE ROUTE
Patient Dose: Codeine elixir 8mg PO q4h : off label use dictates 1mg/kg/dose16kg * 1mg = 16mg/dose which is THEORETICALLY safe for Brittany Long 12 years: Safety and efficacy have not been established; however, doses up to 1 mg/kg/dose (Max: 60 mg/dose) have been used off-label for pain. 1 to 11 years: Use is contraindicated.
PURPOSE FOR TAKING THIS MEDICATION
Management of mild to moderate pain. Antitussive (in smaller doses)
PATIENT EDUCATION WHILE TAKING THIS MEDICATION
Instruct patient on how and when to ask for and take pain medication.
Advise patient that codeine is a drug with known abuse potential. Protect it from theft, and never give to anyone other than the individual for whom it was prescribed.
Instruct patient on risk of addiction, abuse, and misuse, which could lead to death. Discuss safe use, risks, and proper storage and disposal of opioid analgesics with patients and caregivers with each Rx..
May cause drowsiness or dizziness.
Advise patient to change positions slowly to minimize orthostatic hypotension.
Encourage patient to turn, cough, and breathe deeply every 2 hr to prevent atelectasis.
Advise patient that good oral hygiene, frequent mouth rinses, and sugarless gum or candy may decrease dry mouth.
PATIENT EDUCATION WORKSHEET NAME OF MEDICATION, CLASSIFICATION, AND INCLUDE PROTOTYPE
MEDICATION: Morphine sulfate 2 mg IV (o.5 mg/kg/dose) X 1 CLASSIFICATION: o Therapeutic: opioid analgesics o Pharmacologic: opioid agonists PROTOTYPE: Morphine
SAFE DOSE OR DOSE RANGE, SAFE ROUTE Patient Dose: 2mg IV SAFE DOSE: 0.05–0.2 mg/kg every 3–4 hr, maximum: 15 mg/dose. (16kg * 0.05mg ) = 0.8 / (16kg * 0.2mg) = 3.2mg = SAFE DOSE PO Rect: (Adults and Children 1 mo): Prompt-release tablets and solution– 0.2–0.5 mg/kg every 4–6 hr as needed. Controlled-release tablet– 0.3– 0.6 mg/kg every 12 hr. M IV SC (Adults and Children 1 mo): Continuous infusion, postoperative pain– 0.01–0.04 mg/kg/hr. Continuous infusion, sickle cell or cancer pain– 0.02–2.6 mg/kg/hr. IV Neonates: Continuous infusion– 0.01–0.03 mg/kg/hr. Epidural: (Children >1 mo): 0.03–0.05 mg/kg, maximum dose: 0.1 mg/kg or 5 mg/24 hr. Use preservative-free formulation. PURPOSE FOR TAKING THIS MEDICATION
Severe pain (the 20 mg/mL oral solution concentration should only be used in opioid-tolerant patients). Pain severe enough to require daily, around-the-clock long-term opioid treatment and for which alternative treatment options are inadequate (extended release).
Pulmonary edema.
PATIENT EDUCATION WHILE TAKING THIS MEDICATION
Instruct patient how and when to ask for pain medication. Do not stop taking without discussing with health care professional; may cause withdrawal symptoms if discontinued abruptly after prolonged use. Discuss safe use, risks, and proper storage and disposal of opioid analgesics with patients and caregivers with each Rx. May cause drowsiness or dizziness. Caution patient to call for assistance when ambulating Advise patient that morphine is a drug with known abuse potential. Protect it from theft, and never give to anyone other than the individual for whom it was prescribed. Store out of sight and reach of children, and in a location not accessible by others. Advise patient to change positions slowly to minimize orthostatic hypotension. Encourage patients who are immobilized or on prolonged bedrest to turn, cough, and breathe deeply every 2 hr to prevent atelectasis. Home Care Issues: Pedi: Teach parents or caregivers how to accurately measure liquid medication and to use only the measuring device dispensed with the medication. o
Emphasize the importance of aggressive prevention of constipation with the use of morphine
PATIENT EDUCATION WORKSHEET NAME OF MEDICATION, CLASSIFICATION, AND INCLUDE PROTOTYPE
MEDICATION: Docusate sodium 100 mg PO daily (liquid per home dose)
CLASSIFICATION: o Therapeutic Class: agents for atypical mycobacterium, anti-infectives o Pharm. Class: macrolide PROTOTYPE: surfactant,
SAFE DOSE OR DOSE RANGE, SAFE ROUTE X
Patient Dose: Docusate sodium 100 mg PO daily o Recommended dosage is 20–60 mg in 1–4 divided doses SAFE DOSAGE PO (Adults and Children >12 yr): 50–400 mg in 1–4 divided doses. PO (Children 6–12 yr): 40–150 mg in 1–4 divided doses. PO (Children 3–6 yr): 20–60 mg in 1–4 divided doses. PO (Children...
Similar Free PDFs

Brittany Long v SIM Care Plan
- 10 Pages

Charlie Snow v Sim Care Plan
- 7 Pages

Brittany Long Guided Reflection
- 3 Pages

Brittany Long CORE
- 2 Pages

Vsimn brittany long - vsim
- 2 Pages

Long term care - Long
- 4 Pages

Case study 8 Brittany long
- 3 Pages

UTI Care Plan - Care Plan
- 7 Pages

Care plan 3 - Care Plan
- 3 Pages

Care Plan 1 - Care plan
- 7 Pages

Care Plan 2 - Care plan
- 21 Pages

Josephine Morrow v SIm
- 11 Pages

V Sim christopher isbar
- 1 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu


