CDHO Factsheet Atrial Fibrillation PDF
| Title | CDHO Factsheet Atrial Fibrillation |
|---|---|
| Author | Abhishek Sharma |
| Course | Juvenile Justice Procedures |
| Institution | Yavapai College |
| Pages | 4 |
| File Size | 384.4 KB |
| File Type | |
| Total Downloads | 27 |
| Total Views | 171 |
Summary
csad...
Description
Disease/Medical Condition
ATRIAL FIBRILLATION
Date of Publication: August 4, 2017
(also known as “AF” and “a. fib.”)
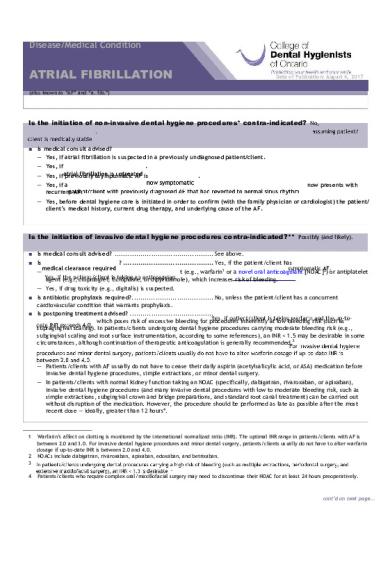
Is the initiation of non-invasive dental hygiene procedures* contra-indicated? No, . ■ Is medical consult advised?
— — — —
Yes, if atrial fibrillation is suspected in a previously undiagnosed patient/client. Yes, if
.
Yes, if previously asymptomatic AF is
.
Yes, if a recurrent AF.
now presents with
— Yes, before dental hygiene care is initiated in order to confirm (with the family physician or cardiologist) the patient/ client’s medical history, current drug therapy, and underlying cause of the AF.
Is the initiation of invasive dental hygiene procedures contra-indicated?** Possibly (and likely). ■ Is medical consult advised? .............................................. See above. ■ Is
—
? .......................................... Yes, if the patient/client has t (e.g., warfarin1 or a novel oral anticoagulant [NOAC]2) or antiplatelet agent (e.g., clopidogrel, ticlopidine, or dipyridamole), which increases risk of bleeding.
— Yes, if drug toxicity (e.g., digitalis) is suspected. ■ Is antibiotic prophylaxis required? ...................................... No, unless the patient/client has a concurrent cardiovascular condition that warrants prophylaxis. ■ Is postponing treatment advised? ....................................... which poses risk of excessive bleeding for procedures inherently at low bleeding risk (such as supragingival scaling). In patients/clients undergoing dental hygiene procedures carrying moderate bleeding risk (e.g., subgingival scaling and root surface instrumentation, according to some references), an INR < 1.5 may be desirable in some circumstances, although continuation of therapeutic anticoagulation is generally recommended. 3
— Patients/clients with AF usually do not have to cease their daily aspirin (acetylsalicylic acid, or ASA) medication before invasive dental hygiene procedures, simple extractions, or minor dental surgery.
— In patients/clients with normal kidney function taking an NOAC (specifically, dabigatran, rivaroxaban, or apixaban), invasive dental hygiene procedures (and many invasive dental procedures with low to moderate bleeding risk, such as simple extractions, subgingival crown and bridge preparations, and standard root canal treatment) can be carried out without disruption of the medication. However, the procedure should be performed as late as possible after the most recent dose — ideally, greater than 12 hours4.
1
2 3 4
Warfarin’s affect on clotting is monitored by the international normalized ratio (INR). The optimal INR range in patients/clients with AF is between 2.0 and 3.0. For invasive dental hygiene procedures and minor dental surgery, patients/clients usually do not have to alter warfarin dosage if up-to-date INR is between 2.0 and 4.0. NOACs include dabigatran, rivaroxaban, apixaban, edoxaban, and betrixaban. . Patients/clients who require complex oral/maxillofacial surgery may need to discontinue their NOAC for at least 24 hours preoperatively.
cont’d on next page...
Disease/Medical Condition
ATRIAL FIBRILLATION (also known as “AF” and “a. fib.”)
Is the initiation of invasive dental hygiene procedures contra-indicated?** (cont’d) — before instrumentation of larger areas is attempted.
— Patients/clients with asymptomatic AF can generally undergo invasive dental hygiene procedures and minor dental surgery in a general practice setting.
Oral management implications ■ An irregular pulse or heartbeat should alert the dental hygienist to the likelihood of atrial fibrillation. Patients/clients with AF are at elevated risk of ischemic events in the dental hygiene/dental office. ■ A stress reduction protocol will minimize the risk of cardiac ischemia5 in the office setting. are generally better for patients/clients with AF, because the risk of an ischemic event is highest during the first few hours of daily activity. ■ Oral sedation (in consultation with physician or dentist) may be appropriate in certain circumstances. If used, an escort should be available to take the patient/client home. ■
(or other vasoconstrictor) is generally recommended for patients/clients with cardiac dysrhythmia or otherwise at risk of cardiac ischemia.
■ Some patients/clients with AF may have memory, language, communication, or attention deficits. In such circumstances, a family member or other caregiver should be included in treatment discussions. ■ Digitalis (e.g., digoxin) is sometimes used in the management of AF. The dental hygienist should be alert to the signs of digitalis toxicity (e.g., anorexia, nausea, vomiting, altered vision, neurologic abnormalities, and facial pain), which should prompt medical referral. ■ Transexamic acid mouth rinse, in addition to application of local pressure, may be used to achieve clotting in patients/clients taking anticoagulants or antiplatelet agents. ■ Because inflammation may be an independent risk factor for the initiation and maintenance of AF, it has been hypothesized that regular dental scaling may lower risk of AF by improving periodontal health. While some studies have shown an association between annual dental scaling and reduced occurrence of new-onset AF, causality has not been proven. Nonetheless, optimal oral hygiene, both in and out of the dental hygiene office, should be promoted.
Oral manifestations ■ There are no oral manifestations caused directly by atrial fibrillation. However, medications used to treat AF may have oral side effects. ■ Anticoagulants (whether warfarin or NOACs) and antiplatelet agents may result in increased and/or prolonged bleeding tendency in the oral cavity.
5
cardiac ischemia = inadequate blood supply to the heart muscles
cont’d on next page...
2
Disease/Medical Condition
ATRIAL FIBRILLATION (also known as “AF” and “a. fib.”)
Oral manifestations (cont’d) ■ Quinidine’s oral side effects include bitter taste, xerostomia, petechiae, and gingival bleeding. ■ Procainamide can cause bitter taste and oral ulcerations. ■ Flecanide can cause metallic taste. ■ Propafenone can cause xerostomia and alteration of taste. ■ Sotalol can cause lichenoid reactions and alteration of taste. ■ Amiodarone can cause alteration of taste. ■ Beta-blockers can cause taste changes. ■ Calcium channel blockers can cause gingival hyperplasia ■ Digoxin can cause excessive salivation.
Related signs and symptoms ■ Atrial fibrillation is the most common sustained cardiac dysrhythmia. It is characterized by rapid uncoordinated contraction of the atria, usually between 350 and 600 times per minute (versus normal range of 60 to 100). The disorganized electrical impulses in the atria6 lead to incomplete atrial emptying, and the ventricles cannot regularly contract in response to the inconsistent impulses. The net effect is increased risk of clot formation, stroke7, myocardial infarction, and heart failure. ■ AF affects about 350,000 Canadians (and between 1% and 2% of the general population worldwide). Prevalence increases with age, reaching 5% to 15% at 80 years. Lifetime risk is about 25%. ■ Risk factors include coronary artery disease, hypertension, heart failure, mitral valve stenosis, hyperthyroidism, hypoxia, and alcohol abuse. Surgery may predispose certain patients/clients to AF. Management consists of either rhythm or rate control 8 — with emphasis on treatment of the underlying cause – as well as drugs specifically directed at reduction of clot formation. ■ The cardinal sign of AF is an irregularly irregular, typically rapid, heartbeat9. AF may be continuous or intermittent. ■ Symptoms of AF include palpitations, light-headedness, shortness of breath, chest pain, and fatigue. However, some persons with AF have no overt symptoms.
6 7 8
9
In a patient/client with AF, an electrocardiogram (ECG) shows no discrete P waves, but rather fine undulations between QRS complexes. 1 in 6 strokes occurs in person with AF. Medical heart rhythm management aims to re-establish normal sinus rhythm (NSR) via one of a variety of anti-arrhythmic agents (e.g., quinidine, procainamide, flecainide, ibutilide, propafenone, sotalol, and amiodarone). Cardioversion (i.e., elective transthoracic delivery of an electric shock) is also used to achieve NSR. Occasionally, cardiac ablation (i.e., a procedure to destroy aberrant conductive heart tissue) may be attempted to restore normal rhythm. Medical heart rate management aims to minimize symptoms and heart damage associated with excessive heart rate via medications such as beta-blockers, calcium channel blockers, and cardiac glycosides (e.g., digitalis/digoxin). Electrophysiological/surgical interventions are also sometimes used to reduce the rapid ventricular rate found in patients/clients with AF. While auscultation of the chest typically reveals a rapid heartbeat (say, 110 beats per minute), not all of these beats may get transmitted to periphery. Thus, the peripheral pulse rate may be slower (say, 90 beats per minute). The difference between the rapid heartbeats and the peripheral pulse (in this example, 20) is known as the pulse deficit of atrial fibrillation.
cont’d on next page...
3
Disease/Medical Condition
ATRIAL FIBRILLATION (also known as “AF” and “a. fib.”)
References and sources of more detailed information ■ CDHO Knowledge Network http://www.cdho.org/Advisories/CDHO_Factsheet_Post-MI.pdf ■ 2016 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation. Can J Cardiol. 2016;32:1170-1185. http://www.onlinecjc.ca/article/S0828-282X(16)30829-7/pdf ■ Tsolka P. Dental Procedures in Patients with Atrial Fibrillation and New Oral Anticoagulants. Arrhythm Electrophysiol Rev. 2014 Aug;3(2):85-89. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4711592/ ■ Humber C. Point of Care – A patient new to my practice has atrial fibrillation. How should I modify the patient’s regular dental care in light of this condition? JCDA. 2005 Nov;71(10):735-736. http://www.cda-adc.ca/jcda/vol-71/issue-10/735.pdf ■ Camm AJ, Savelieva I and Lip GYH. Rate control in the medical management of atrial fibrillation. Heart. 2007 Jan;93 (1):35-38. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1861356/ ■ Thrombosis Canada www.thrombosiscanada.ca ■ Heart and Stroke Foundation of Canada https://www.heartandstroke.ca/heart/conditions/atrial-fibrillation ■ Dentistry IQ http://www.dentistryiq.com/articles/2013/04/atrial-fibrillation.html ■ RDH Magazine (same article as Dentistry IQ article above) http://www.rdhmag.com/articles/print/volume-33/issue-8/features/atrial-fibrillation-link-to-oral-disease.html ■ Canadian Dental Association https://www.cda-adc.ca/_files/position_statements/infectiousEndocarditis.pdf ■ Darby M (ed.) and Walsh M (ed.). Dental Hygiene: Theory and Practice (4 th edition). St. Louis: Elsevier Saunders; 2015. ■ Little JW, Falace Da, Miller CS and Rhodus NL. Dental Management of the Medically Compromised Patient (8 th edition). St. Louis: Elsevier Mosby; 2013. *
Includes oral hygiene instruction, fitting a mouth guard, taking an impression, etc.
** Ontario Regulation 501/07 made under Dental Hygiene Act, 1991. Invasive dental hygiene procedures are scaling teeth and root planing, including curetting surrounding tissue.
Date: June 12, 2017
69 Bloor St. E, Suite 300, Toronto, ON M4W 1A9 t: 416-961-6234 ● tf: 1-800-268-2346 ● f: 416-961-6028 ● www.cdho.org
4...
Similar Free PDFs

Atrial Fibrillation system
- 1 Pages

ACDC Factsheet
- 2 Pages

LP ATRIAL FIBRILASIS AF
- 22 Pages

Muscle Fibrillation
- 4 Pages

Factsheet - gjbkjhlihlijp
- 3 Pages

Evicting a tenant factsheet
- 1 Pages

Fines-understanding-factsheet
- 2 Pages

Sobrecarga Atrial - ECG
- 2 Pages

Swift Standards Factsheet SR2016
- 11 Pages

Alcohol Factsheet Headspace-1
- 2 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu





