Fsmith answers Simulation Case Study PDF
| Title | Fsmith answers Simulation Case Study |
|---|---|
| Course | Mental-Health Nursing |
| Institution | Chamberlain University |
| Pages | 4 |
| File Size | 78.2 KB |
| File Type | |
| Total Downloads | 106 |
| Total Views | 147 |
Summary
The F Smith case study for Simulation Lab in class assignment....
Description
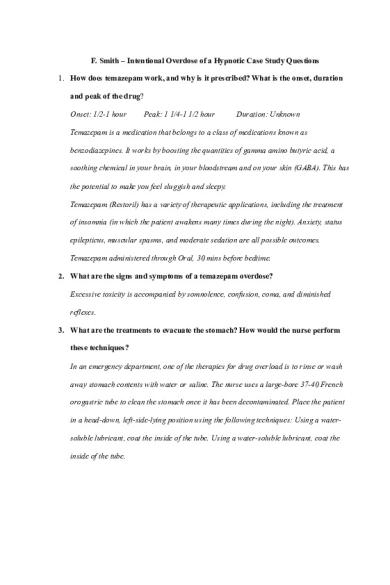
F. Smith – Intentional Overdose of a Hypnotic Case Study Questions 1. How does temazepam work, and why is it prescribed? What is the onset, duration and peak of the drug? Onset: 1/2-1 hour
Peak: 1 1/4-1 1/2 hour
Duration: Unknown
Temazepam is a medication that belongs to a class of medications known as benzodiazepines. It works by boosting the quantities of gamma amino butyric acid, a soothing chemical in your brain, in your bloodstream and on your skin (GABA). This has the potential to make you feel sluggish and sleepy. Temazepam (Restoril) has a variety of therapeutic applications, including the treatment of insomnia (in which the patient awakens many times during the night). Anxiety, status epilepticus, muscular spasms, and moderate sedation are all possible outcomes. Temazepam administered through Oral, 30 mins before bedtime. 2. What are the signs and symptoms of a temazepam overdose? Excessive toxicity is accompanied by somnolence, confusion, coma, and diminished reflexes. 3. What are the treatments to evacuate the stomach? How would the nurse perform these techniques? In an emergency department, one of the therapies for drug overload is to rinse or wash away stomach contents with water or saline. The nurse uses a large-bore 37-40 French orogastric tube to clean the stomach once it has been decontaminated. Place the patient in a head-down, left-side-lying position using the following techniques: Using a watersoluble lubricant, coat the inside of the tube. Using a water-soluble lubricant, coat the inside of the tube.
Insert the tube approximately 20 inches nasogastric or orogastric. Tape the tube to the ground to keep it in place. Before administering the solution, aspirate the stomach contents with a syringe. Keep the specimen safe. Install 50-100 standard saline or water and aspirate the contents regularly. Continue to repeat the procedure until the stomach return is clean. 4. What drug antagonist may be used to treat benzodiazepine overdoses? What is the dosage in adults? What is the risk or complication with its use? To reverse the symptoms of pure benzodiazepine overdose with flumazenil is the best option. The sedative can cause respiratory depression effects. Flumazenil dose for adults is as follows: The first dose was 0.2mg IV/IO given over 15 seconds, the second dose was 0.3mg delivered over 30 seconds, and the third dose was 0.5mg given over the same time. Flumazenil can cause the following adverse reactions/side effects: seizures, dizziness, agitation, confusion, headache, visual disturbances, dysrhythmias, chest pain, hypertension, nausea, vomiting, hiccups, rigor, shivering, and pain at the injection site. 5. Discuss the nursing interventions to be utilized with a family member who is in crisis in the care setting and interfering with the healthcare team’s performance. Ensure that you are working on creating a therapeutic relationship with the patient's family. Gathering them in a private space and inviting them to share what they are concerned about.
6. Describe nursing communication techniques utilized in crisis situations with families. Remember to be patient; the most essential thing is to pay attention and pay attention well. Even if their arguments appear unreasonable or unjustified, refrain from becoming defensive. Explain that their thoughts and expertise about the patient are valuable and will be used to give the best possible care. 7. Identify the patient’s suicidal behavior from the terms listed below. Explain each term and the behavior that would indicate its presence. Suicide attempt- The act of self-mutilation suggests that it is now taking place. A potentially life-threatening self-injurious incident or behavior with a nonfatal outcome in which there is evidence that the subject had at least some intent to die. Suicidal gestures - A range of behaviors can be used to transmit the message of suicide intent and cause little or no hurt. Suicidal ideation - Thoughts or fancies that are not accompanied by a clear intention— may express concepts directly or symbolically. The patient may express a desire to die or believe that they do not wish to live any longer. Suicidal intent - To have the intention of committing suicide or deliberately selfimmolating as a goal. Suicidal threats - Expressions of intent, whether verbal or written, that are not followed by action 8. What factors might have contributed to the patient’s suicide attempt? Widowed individuals with a psychological disease of Caucasian ethnicity and over 65 years old are common factors for suicide.
9. How serious do you think the patient is about dying? Why? Although the patient has left the service, their risk of suicide continues to be high because of a previous suicide attempt, advanced age, and the death of a loved one, all of which increase the patient's risk of suicide. 10. Should the nurse speak with the patient about suicide? Why or why not? If the patient specifically mentions suicide, the nurse should inquire as to whether she is experiencing any thoughts of killing herself by asking the patient directly. If a nurse asks simple questions such as "Do you want to damage yourself?" and "Do you want to kill yourself?" it is critical that the patient responds positively. The nurse should offer to the patient that he or she be placed under 1:1 surveillance if the patient responds affirmatively. 11. To what unit will this patient be admitted? Why? The patient has been admitted to a psychiatric facility. Typically, the client is brought to the unit for 5-7 days, or until the patient indicates that she no longer wishes to try suicide or that she wishes to live. a. What are the HIPAA guidelines and regulations regarding a patient’s family member in an emergency situation? If a patient is unable to communicate with his or her family members, friends, or other individuals who are involved in the patient's health care or payment for care, health care providers may communicate with those individuals if the patient is unable to communicate with all of the individuals listed above....
Similar Free PDFs

Case Study with answers
- 6 Pages

Depression case Study Answers
- 2 Pages

Hygiene Case study answers
- 3 Pages

Case study - answers
- 1 Pages

Kate Spade Case Study Answers
- 17 Pages

Answers to Case Study 1
- 3 Pages

Module 3 Case Study Answers
- 6 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu








