HNN222- Week 1 Introduction to mental health and illness, and mental health nursing: PDF

| Title | HNN222- Week 1 Introduction to mental health and illness, and mental health nursing: |
|---|---|
| Course | Nursing |
| Institution | Deakin University |
| Pages | 13 |
| File Size | 226.5 KB |
| File Type | |
| Total Downloads | 30 |
| Total Views | 143 |
Summary
Download HNN222- Week 1 Introduction to mental health and illness, and mental health nursing: PDF
Description
HNN222: Week 1 Introduction to mental health and illness, and mental health nursing: Intended learning outcomes: Define mental health and illness Discuss the impacts of stigma and stereotyping on people experiencing mental health difficulties Describe the key elements of mental health nursing practice Discuss the concepts of person-centred care and therapeutic communication as they apply to mental health nursing Define biopsychosocial model of care as it relates to mental health nursing Develop understanding of the concept of recovery including its definition, enablers and barriers to recovery Develop beginning understanding of trauma and its impact on mental wellbeing; reflect on the role of the nurse in delivering trauma-informed practice. Develop beginning understanding of psychopathology & psychopharmacology
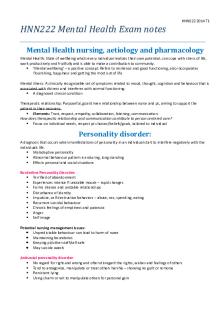
Define mental health and illness: Mental health: state of wellbeing where every individual realises their own potential, can cope with stress of life, work productively and is able to contribute to the community. - our ability to respond and cope with life’s challenges - state of mind that allows you to cope with challenges which can be eroded by risk factors or supported by protective factors Risk factors and protective factors of mental health: Risk: - chronic illness - low socioeconomic status Protective: can help shape someone’s mental health across a lifespan - supportive family - self efficacy - strong friendship Mental illness: Clinically recognizable set of symptoms related to mood, thought, cognition and behaviour that is associated with distress and interferes with normal functioning. - a diagnosed clinical condition - a health problem that significantly affects how a person feels, thinks, behaves, and interacts with other people. - chronic disruptions in the neural circuits of the brain which affect the functioning of the brain Biological and environmental factors include: - Genetics (inherited susceptibility - Traumatic events - Stress - Drugs and alcohol - Lack of sleep Disrupted neural circuits can be helped by: - Psychiatric treatment - Effective therapy - Peer support - Family support - Sleep, diet and exercise How does mental health differ from mental illness?
- Everyone has mental health - Not everyone will experience mental illness - Mental health – wellbeing, emotions, thoughts, feelings, ability to solve problems and overcome difficulties, social connections, understanding of the world. - Mental illness – affects the way we think, feel, behave and interact. - Mental illness includes a wide range of conditions such as bipolar disorder, schizophrenia, eating disorders. - Mental health is along a continuum. Is there such a thing as normal? How do we define ‘normal’ - “the usual, typical or expected state or condition” - Everyone’s normal is different - Very subjective Types of mental illnesses: - anxiety - depression - schizophrenia - bipolar disorder - OCD - ADHD - clinical depression - Autism
Discuss the impacts of stigma and stereotyping on people experiencing mental health difficulties: Stigma: a mark of disgrace associated with particular circumstances, quality or person - which sets a person apart. - when a person is labelled by their illness they are seen as part of a stereotyped group - negative attitudes create prejudice, which leads to negative actions and discrimination - Stigma and stereotyping have shown to have the potential to contribute to the degree of disability experienced by a person who is ill or recovering from illness - the stigma from a mental illness can stop people from accessing services Commonly held misconceptions.. All people with mental disorders - are violent and dangerous - have an intellectual disability or brain damage - will never recover - decreased functioning - Schizophrenia: patients have split personality - there is a strong relationship between individuals not seeking help regarding mental illness due to a lack of understanding and education regarding mental health, other factors including fear, stigma, lack of access to health care - social determinants strongly influence mental health - Dangerous - Crazy - Incompetent - disabled - untrustworthy What impact might stigma have on someone experiencing a mental illness? - A person who is stigmatised may be treated differently and excluded from many things the rest of society takes for granted. - People with mental illness may also take on board the prejudiced views held by others, which can affect their self-esteem. This can lead them to not seek treatment, to withdraw from society, to alcohol and drug abuse or even to suicide.
Describe some key elements of mental health nursing practice: - recognise the persons rights - deliver evidence based client centred care - deliver services with the aim to facilitate sustained recovery - learn about and value the lived experience of people using services, and their family or carers - tailor mental health care to the individual What are the essential skills and knowledge required in mental health nursing? - Knowledge of mental illness - Active listening - Empathy - Reflective practice - Observation - Patient assessment - Problem solving ability - Humour - Assertiveness - Communication/respect 1) Compassion and care: - sensitivity to suffering and a desire to alleviate distress - being accepting and non judgemental attitude, being present and listening - put yourself in patient’s shoes 2) Hope and spirituality: - Hope is considered essential in handling illness - described as the act by which the temptation to despair is actively overcome - big relationship to health, mental wellbeing and recovery from illness or traumatic life events 3) Therapeutic use of self: therapeutic relationships provide healing connections through caring, emotional connection and narrative and anxiety management 4) Self awareness: lack of self awareness can cause nurses to respond to a clients distress and behaviour in ways that may not be helpful 5) Reflection:critically reviewing experience from practice to change and inform future practice 6) Professional boundaries: coercion, use of force, over treatment or under treatment or inappropriate intimate relationships
Standards of practice in mental health nursing: - provide practical benchmarks to guide and measure how care is provided - they are concerned with the performance of mental health nurses across a range of clinical environments and include professional knowledge, skills and attitudes (attributes). - the ACMHN standards of practice for Australian mental health nurses 2010 specify the minimum level of performance required for a registered nurse practising in any mental health setting The 9 standards: Standard 1: The mental health nurse acknowledges diversity in culture, values and belief systems and ensures his/her practice is non-discriminatory, and promotes dignity and self-determination. Standard 2: The mental health nurse establishes collaborative partnerships that facilitate and support people with mental health issues to participate in all aspects of their care. Standard 3: The mental health nurse develops a therapeutic relationship that is respectful of the individual’s choices, experiences and circumstances. This involves building on strengths, holding hope and enhancing resilience to promote recovery. Standard 4: The mental health nurse collaboratively plans and provides ethically based care consistent with the mental, physical, spiritual, emotional, social and cultural needs of the individual. Standard 5: The mental health nurse values the contributions of other agencies and stakeholders in the collaborative provision of holistic, evidence based care and in ensuring comprehensive service provision for people with mental health issues. Standard 6: The mental health nurse actively pursues opportunities to reduce stigma and promotes social inclusion and community participation for all people with mental health issues. Standard 7: The mental health nurse demonstrates evidence based practice and actively promotes practice innovation through lifelong education, research, professional development, clinical supervision and reflective practice. Standard 8: The mental health nurse’s practice incorporates and reflects common law requirements, relevant statutes and the nursing profession’s code of conduct and ethics. The mental health nurse integrates international, national, local and state policies and guidelines with professional standards and competencies. Standard 9: The mental health nurse holds specialist qualifications and demonstrates advanced specialist knowledge, skills and practice, integrating all the standards competently and modelling leadership in the practice setting.
Discuss the concepts of person-centred care and therapeutic communication as they apply to mental health nursing Person centred care: It ensures that the patient is at the centre of the decision making process to ensure satisfaction and promote better outcomes List as many components of PCC as you can think of - Self-management support - Shared Decision Making/collaboration - Digital health - refers to different range of technologies - Health literacy - patients understanding - Integrated Care - Personalised care & support planning - Personal Health Budget - Records access - Advocacy Explain why PCC is important to safe high quality mental health care It allows the patient feel like they have some sort of control or power over their illness. Compare the principles of PCC and recovery focused care - Shared values of respecting patient choices - Partners in care planning & delivery, participation, collaboration What is ‘therapeutic relationship’? - Relationship where the nurse and patient work together towards meet life challenges and facilitate growth. What are the core elements of a therapeutic relationship? - trust - Warmth - Empathy - Understanding - Acceptance - Genuineness - Kindness How does therapeutic communication and the therapeutic relationship contribute to person centred care? - nurses require highly developed communication and interpersonal skills to enable and nurture a therapeutic relationship - Good communication between nurses and patients is the goal of assisting the patient to regain the inner resources to for the successful outcome of individualized nursing care of each essential patient
What are some enablers to effective therapeutic relationships? - Background knowledge - Knowledge of interpersonal, caring and development - Knowledge of culture, diversity and determinants of health - Knowledge of patient - Knowledge of health/illness - Knowledge of systems - Empathy - Self-awareness - Self-knowledge - Awareness of ethics, boundaries and professional roles - Caring What are some potential barriers to effective therapeutic relationships? - Ineffective communication - Judgmental statements - Blaming - Demanding - Dishonest - Over-catastrophising statements - Lack of trust - Hostile relationship
Define biopsychosocial model of care as it relates to mental health nursing: Biopsychosocial model definition: an approach to describing and explaining how biological, psychological and social factors combine and interact to influence physical and mental health.
Case study: Jenni is a 23 year old woman who arrived at ED with a friend after falling over and sustaining a deep laceration to her arm. On arrival she appeared to be intoxicated, distressed and tearful. On examination she admitted to use ketamine and alcohol at a club, but added she does not usually use drugs, but the past month she has been ‘out of control’ since breaking up with her BF. She describes feeling depressed, unable to work, poor appetite and sleep for the past 2 weeks. BIO: Medication, harm minimisation, referral drug/alcohol service Psycho: Support, reassurance, mental health assessment, counselling Social: referral to social support, employment assistance, youth mental health services
Develop understanding of the concept of recovery and identify enablers and barriers to recovery in the mental health setting: Recovery: - Recovery oriented practice is an integral part of mental health nursing. In mental health, recovery!is not just focused on recovery from illness, but involves many factors including finding and maintaining hope; autonomy and self determination; collaboration between consumers and mental health professionals; involvement of family and important support networks; citizenship and social inclusion; finding purpose and meaning in life; provision of holistic care; and focusing on the person's strengths. - Recovery is therefore a unique and individual experience and is defined by the person Definition: ‘A deeply personal, unique process of changing one’s attitudes, values, goals, skills and/or roles. It is a way of living a satisfying, hopeful and contributing life even within the limitations caused by the illness. Recovery involves the development of new meaning and purpose in one’s life as one grows beyond the catastriphic effects of mental health’. Enablers to a therapeutic relationship: Trust: - critical in the nurse-patient relationship as patient is in a vulnerable position - once breached, it becomes very difficult to re-establish Respect: - is the recognition of the inherent dignity, worth and uniqueness of everyone regardless of SES, personal attributes and nature of the health problem Professional intimacy: - is essential in the type of care and services nurses provide - related to physical activities (such as bathing), psychological, spiritual and social elements. Empathy: - is the expression of understanding, validating and resonating with the meaning that the health care experience holds for the patient - includes appropriate emotional distance to ensure objectively and appropriate professional responses Power: - patient nurse relationships is one of unequal power - nurses have more power, authority, influence, specialised knowledge, access to privileged information and ability to advocate for the patients and their loved one - appropriate use of power in a caring manner enables nurse to partner with patient
- a misuse of power is considered abuse Therapeutic communication: - establishes, maintains and re-establishes the nurse patient relationship - address with name/title (not darl, love ect) - inform patient - introduce yourself Client-centred care: - nurses work with the client to ensure that all professional behaviours and actions meet the therapeutic needs of the client Maintaining boundaries: - nurses are responsible for effectively establishing and maintain the limits or boundaries in the therapeutic nurse patient relationship Barriers to a therapeutic relationship: - cold and distant - lack of trust - abuse - miscommunication - lack of sympathy What are some potential barriers to effectively implement recovery focused care? - communication - stigma - environment - discrimination - unemployment - lack of therapeutic relationship - lack of self determination - unable to value themselves as a person through their interactions with others - patient not wanting to recover - unable to explore experiences with reference to both the present and the future self - unable to find ways to monitor and manage the symptoms of distress - lack of optimism - lack of service engagement Provide some examples of practices in health and nursing care that may support recovery: - education - collaborative partnerships: health professionals, families, friends - shared decision making - peer support
- collaborative crisis planning - mental health promotion - trauma informed (“what happened to you”) - need to create a space where they can open up - affirmation - resources: housing, food, transport, stable income Health providers
People with lived experiences of mental illness
Chronic
In recovery
Symptoms
Experiences
High/low functioning
Having a good/bad day
Manipulative
Strategic
My client/patient
People I work with
Referred to be diagnosis
Person
The mentally ill
People
Non-compliant
Non in agreement with me
Treatment resistance
Considering other options
Safety and risk
Feeling supported enough to try new thing dignity of managing self
Decompensated
Having a bad day
Develop beginning understanding of trauma and its impact on mental wellbeing; reflect on the role of the nurse in delivering trauma-informed practice What is Trauma Informed Care? Definition: Trauma informed!practice recognises the impact of trauma and the interplay between trauma and!mental health. A key aspect of trauma informed!practice is providing a safe environment for people who have a history of trauma. Trauma-informed care is a term that people working in youth mental healthcare are likely to be familiar with but may struggle to define. Trauma-informed care can seem conceptual rather than practical, and definitions of trauma-informed care often vary. This can make it difficult to pinpoint what it should look like in youth healthcare settings, and what policymakers, service managers, and staff should be doing to support its implementation. - ‘A program, organisation, or system that is trauma-informed: - Realises the widespread impact of trauma and understands potential paths for recovery. - Recognises the signs and symptoms of trauma in clients, families, staff, and others involved with the system. - Responds by fully integrating knowledge about trauma into policies, procedures, and practices. - Seeks to actively resist re-traumatization.’ Core principles of trauma-informed care within youth healthcare settings: - Safety - Trustworthiness and transparency - Collaboration and mutuality - Empowerment - Voice and choice - Culture, historical and gender issues...
Similar Free PDFs

Nursing and Mental Health 1 Notes
- 62 Pages

Uworld Mental Health Nursing
- 168 Pages

Week 1 Mental Health ATI
- 11 Pages

ebook for mental health nursing
- 219 Pages

Social Media and Mental Health
- 9 Pages

ATI TEST - mental health nursing
- 38 Pages

Mental Health
- 44 Pages

Mental health quiz 1
- 2 Pages

WEEK 26 Mental Health Update
- 8 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu