Med Surg- Care Plan PDF

| Title | Med Surg- Care Plan |
|---|---|
| Course | Medical surgical |
| Institution | ECPI University |
| Pages | 6 |
| File Size | 196 KB |
| File Type | |
| Total Downloads | 12 |
| Total Views | 161 |
Summary
Download Med Surg- Care Plan PDF
Description
NUR 322 Nursing Care of the Adult Clinical
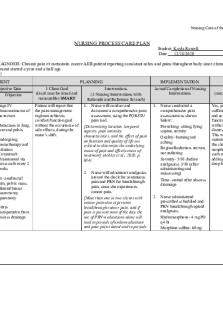
NURSING PROCESS CARE PLAN Student Kayla Rowell Date 12/18/2020 NURSING DIAGNOSIS: Chronic pain r/t metastatic cancer AEB patient reporting consistant aches and pains throughout body since chemotherapy and radiation treatment started a year and a half ago PRIORITY # 1 ASSESSMENT Subjective and Objective Data Subjective Objective Chief complaint“buttocks pain” “I am in so much pain when sitting, so I need to stand or lay on my side”
Stage IV adenocarcinoma of the rectum Metastases to lung, liver and pelvis Undergoing chemotherapy and radiation -Cetuximab administered via port-a-cath every 2 weeks Hx- anal/rectal pain, pelvic mass, bilateral breast mastectomy, laparotomy 4 days postoperative from abscess drainage
10/2017rmr
PLANNING Interventions (3 Nursing Interventions with Rationale and Reference for each)
1 Client Goal (Goal must be timed and measurable) SMART Patient will report that the pain management regimen achieves comfort-function goal without the occurrence of side effects, during the nurse’s shift.
1.
Nurse will conduct and document a comprehensive pain assessment, using the PQRSTU pain tool. [Determining location, temporal aspects, pain intensity, characteristics, and the effect of pain on function and quality of life are critical to determine the underlying cause of pain and effectiveness of treatment] (Ackley et al., 2020, p. 684) Nurse will administer analgesics around the clock for continuous pain and PRN for breakthrough pain, since she experiences cancer pain. [More than one in two clients with cancer pain also experience breakthrough cancer pain, and if pain is present most of the day, the use of PRN medications alone will lead to periods of undermedication and poor pain control and to periods
IMPLEMENTATION Actual Completion of Nursing Interventions 1.
Nurse conducted a comprehensive pain assessment as shown below: Provoking- sitting, lying supine, activity Quality- burning and aching Region/Radiation- rectum, not radiating Severity- 5/10 (before analgesics) 3/10 (after administering and reassessing) Time- started after abscess drainaige
2.
2.
Nurse administered prescribed scheduled and PRN breakthrough opioid analgesics. Hydromorphone- 4 mg PO q4 hr Morphine sulfate- 60mg
EVALUATION Goal Evaluation (met, not met, partially met and explanation) Yes, patient reported sufficient pain management and achieved comfortfunction goal of a 3/10 without any respiratory distress or other side effects. This was accomplished by maintaining routine around the clock analgesics and using nonpharmacological methods, such as position changes, adding extra pillows, and deep breathing exercises.
NUR 322 Nursing Care of the Adult Clinical
of excessive medication and adverse effects] (Ackley et al., 2020, p. 686) 3. In addition to administering analgesics, nurse will teach and educate the patient on nonpharmacological methods to help control pain. [Evidence suggested efficacy and satisfaction when complementary therapies are integrated into pain treatment plans of adults] (Ackley et al., 2020, p. 687) * Cite all interventions/rationales per APA format
10/2017rmr
3.
PO q12 hr (PRN) Acetaminophen- 500 mg PO q4-6 hr (PRN) Nurse taught patient nonpharmacological methods to help control pain. These included- deep breathing exercises, position changes, and additional pillows for comfort. Nurse also used the distraction technique when in patient’s room.
NUR 322 Nursing Care of the Adult Clinical
NURSING DIAGNOSIS: Impaired oral mucous membrane integrity r/t chemotherapy AEB patient states, “I use Magic Mouthwash for my painful mouth sores” PRIORITY # 2 ASSESSMENT Subjective and Objective Data Subjective Objective “My mouth sores are causing me pain and discomfort” “Sometimes the sores make it difficult to swallow and ingest certain foods”
“I use Magic Mouthwash for my painful mouth sores”
Stomatitis- oral mucositis Ulcerations currently visible: - 3 on tongue - 1 on lip - 2 on roof of mouth Fluid intake- 2,600 mL (12/11) Xerostomia
PLANNING 1 Client Goal (Goal must be timed and measurable) SMART Patient will demonstrate measures to regain intact oral mucous membranes, during the nurse’s shift.
Interventions (3 Nursing Interventions with Rationale and Reference for each) 1. Nurse will inspect the patient’s oral cavity and document the presence and severity of stomatitis. [Inspection is a critical diagnostic tool; observations can identify impending problems] (Ackley et al., 2020, p. 658) Nurse will provide Magic Mouthwash, a systemic and/or topical analgesic as PRN prescribed to help relieve oral mucositis symptoms. [This will provide comfort and relieve pain] (Ackley et al., 2020, p. 660)
IMPLEMENTATION Actual Completion of Nursing Interventions 1.
Nurse assessed patient’s mouth and noted the presence of stomatitis. Patient’s mouth sores seemed to be healing due to her chemotherapy cycle being postponed until she healed from recent surgery. Her counts were able to go back up.
2.
Nurse provided Magic Mouthwash (30 mL q4-6 hrs PO- swish in mouth for 1 minute then spit out, do not rinse) to patient upon request when she was experiencing stomatitis discomfort.
2.
3.
Nurse will monitor patient’s fluid status and encourage fluid intake (up to 3000 mL/day) to ensure adequate hydration and help protect mucous membranes. [Fluids help increase moisture in the mouth, which protects the mucous membranes from damage] (Ackley et
10/2017rmr
0800- 30 mL 1300- 30 mL 1800- 30 mL
3.
Nurse monitored patient’s fluid status and encouraged fluid intake for
EVALUATION Goal Evaluation (met, not met, partially met and explanation) Yes, patient demonstrated measures to regain intact oral mucous membranes during the nurse’s shift. This included maintaining adequate hydration and using a Magic Mouthwash rinse to alleviate pain/discomfort and promote healing. Fluid intake during shift2,600 mL
NUR 322 Nursing Care of the Adult Clinical
al., 2020, p. 659)
hydration of mucous membranes. This helped increase moisture and protection in the mouth.
* Cite all interventions/rationales per APA format
NURSING DIAGNOSIS: Risk for infection AEB compromised immune system from prolonged chemotherapy treatment PRIORITY # 3 ASSESSMENT Subjective and Objective Data Subjective
Objective Stomatitis- oral mucositis Currently undergoing chemotherapy treatment BP0800: 122/66 1200: 113/74 1600: 110/65 HR0800: 104 1200: 98 1600: 76 RR0800: 18 1200: 16 1600: 16 T0800: 98.2 1200: 97.8 1600: 97.9 WBC- 5.6
10/2017rmr
PLANNING Interventions (3 Nursing Interventions with Rationale and Reference for each)
1 Client Goal (Goal must be timed and measurable) SMART Patient will remain free of infection, as evidenced by normal vital signs and absence of signs and symptoms of infection, throughout the nurse’s shift.
1.
Nurse will assess and report any redness, warmth, purulent exudate, and increased body temperature experienced by patient. [These factors represent a break in the body’s normal first line of defense and may indicate an infection] (Ackley et al., 2020, p. 547) Nurse will ensure the client's appropriate hygienic care with handwashing; bathing; oral care; and hair, nail, and perineal care performed by either the nurse or the patient. [Daily showers or baths can help to reduce the number of bacteria on the client's skin. The oral cavity is a common site for infection.] (Ackley et al., 2020, p. 549)
IMPLEMENTATION Actual Completion of Nursing Interventions 1.
Nurse assessed for any signs of an infection such as redness, warmth, purulent exudate, and increased of temperature. No presence of infection during shift. Temperature- 0800: 98.2; 1200: 97.8; 1600: 97.9
2.
3.
Nurse will follow standard precautions by foaming in and out of patient room, and wearing
2.
Nurse ensured appropriate hygiene measures. During shift, nurse witnessed patient washing hands often, take a shower by self, and brush teeth twice. This helped reduce patient’s risk of developing infection by minimizing bacteria on skin.
3.
Nurse followed standard precautions and wore gloves when in contact
EVALUATION Goal Evaluation (met, not met, partially met and explanation) Yes, patient remained free of infection, as evidenced by normal vital signs and absence of s/s of infection.
NUR 322 Nursing Care of the Adult Clinical
Imm. gran. abs0.10 (low) Lymph abs- 0.5 (low) Seg. Neutrophil83 (high) Lymphocytes- 5 (low) Monocytes- 10 (high) Myeloctes- 2 (high) RBC- 2.9 (low) Hmg- 7.9 (low)
gloves during any contact with blood, mucous membranes, nonintact skin, or any bodily substance. [Hands of health care workers are the most common cause of health care–associated infections] (Ackley et al., 2020, p. 548)
* Cite all interventions/rationales per APA format
10/2017rmr
with bodily fluids. This helped prevent the spread of nosocomial infections the patient could have potentially developed during hospital stay.
NUR 322 Nursing Care of the Adult Clinical
References Ackley, B. J., Ladwig, G. B., Flynn Makic, M. B., Martinez-Kratz, M.R., & Zanotti, M. (2020). Nursing diagnosis handbook: An evidence-based guide to planning care. (12th ed.). Elsevier.
10/2017rmr...
Similar Free PDFs
Med Surg- Care Plan
- 6 Pages

Med surg 2 care plan
- 3 Pages

Common Med Surg Meds
- 7 Pages

Med surg dorris bowman
- 4 Pages

Med surg - notes
- 28 Pages

Med-Surg Endocrine
- 11 Pages

Med-Surg Capstone remediation
- 4 Pages

Med Surg Exam 3
- 19 Pages

Kaplan med surg 2
- 8 Pages

Med surg 1
- 33 Pages

med surg review questions
- 7 Pages

Adv med surg remediation
- 2 Pages

Med SURG; assignment 2
- 9 Pages

Med Surg ATI Remediation
- 6 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu

