NR 509 SOAP Note Week 4 PDF
| Title | NR 509 SOAP Note Week 4 |
|---|---|
| Course | Advanced Physical Assessment |
| Institution | Chamberlain University |
| Pages | 10 |
| File Size | 1 MB |
| File Type | |
| Total Downloads | 35 |
| Total Views | 143 |
Summary
Download NR 509 SOAP Note Week 4 PDF
Description
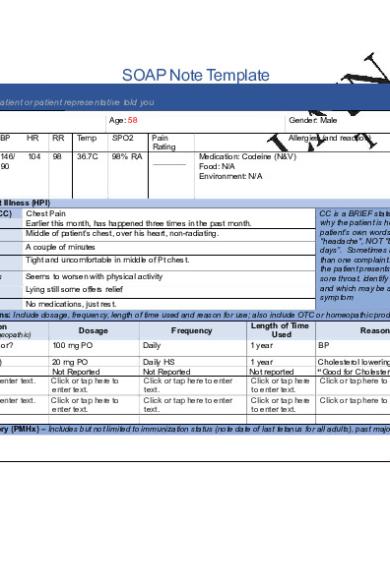
SOAP Note Template S: Subjective Information the patient or patient representative told you Initials: BF
Age: 58
Height
Weight
BP
HR
RR
Temp
SPO2
5’11”
197 lbs
146/ 90
104
98
36.7C
98% RA
Gender: Male Pain Rating
Allergies (and reaction) Medication: Codeine (N&V) Food: N/A Environment: N/A
History of Present Illness (HPI) Chief Complaint (CC) Chest Pain Onset Earlier this month, has happened three times in the past month. Location Middle of patient’s chest, over his heart, non-radiating. Duration
A couple of minutes
Characteristics
Tight and uncomfortable in middle of Pt chest.
Aggravating Factors
Seems to worsen with physical activity
Relieving Factors
Lying still some offers relief
CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom
Treatment No medications, just rest. Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Length of Time Medication Dosage Frequency Reason for Use (Rx, OTC, or Homeopathic) Used Metoprolol (Lopressor? 100 mg PO Daily 1 year BP Atorvastatin (Lipitor) Omega 3 Fish OIL Click or tap here to enter text. Click or tap here to enter text.
20 mg PO Not Reported Click or tap here to enter text. Click or tap here to enter text.
Daily HS Not Reported Click or tap here to enter text. Click or tap here to enter text.
1 year Cholesterol lowering medication Not reported “Good for Cholesterol” Click or tap here Click or tap here to enter text. to enter text. Click or tap here Click or tap here to enter text. to enter text.
Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses,
hospitalizations, and surgeries. Depending on the CC, more info may be needed.
Patient reports being up to date on all immunizations and confirms all allergies. Pt denies any previous hospitalizations or surgeries. Patient denies previous diagnosis of angina, CAD, DM, or previous chest pain treatment. Pt positive history for HTN and elevated cholesterol. Reports infrequent BP monitoring at home, reports recent EKG test and annual stress test as “normal”.
Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. The patient reports a generally low stress lifestyle, employed at a civil engineering firm in town. Patients diet consists of grilled meats (typically red meat, 4-5 times a week), sandwiches, and vegetables, Pt drinks 1-2 cups of coffee a day, denies tobacco use, reports alcohol use at 2-3 drinks a week, typically in one sitting. Denies soda consumption, drinks 4 glasses of water/day, denies regular exercise routine.
Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Pt reports family history of heart attack, maternal grandfather deceased from heart attack at young age. Father dies of colon cancer, Mother and Sister have DM, Daughter has asthma, and all family members have elevated BP. Denies family history of Stroke or PE.
Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details.
Constitutional If patient denies all symptoms for this system, check here: ☒ ☐Fatigue Denies ☐Weakness Denies ☐Fever/Chills Denies ☐Weight Gain Denies ☐Weight Loss Denies ☐Trouble Sleeping Denies ☐Night Sweats Denies ☐Other: Click or tap here to enter text.
Skin If patient denies all symptoms for this system, check here: ☐ ☐Itching Click or tap here to enter text. ☐Rashes Click or tap here to enter text. ☐Nail Changes Click or tap here to enter text. ☐Skin Color Changes Click or tap here to enter text. ☐Other: Click or tap here to enter text.
Respiratory If patient denies all symptoms for this system, check here: ☒ ☐Cough Denies ☐Hemoptysis Denies ☐Dyspnea Denies ☐Wheezing Denies ☐Pain on Inspiration Denies ☐Sputum Production
☐Other: Click or tap here to enter text.
HEENT If patient denies all symptoms for this system, check here: ☐
☐Diplopia Click or tap here to enter text. ☐Eye Pain Click or tap here to enter text. ☐Eye redness Click or tap here to enter text. ☐Vision changes Click or tap here to enter text. ☐Photophobia Click or tap here to enter text. ☐Eye discharge Click or tap here to enter text.
Neuro If patient denies all symptoms for this system, check here: ☐ ☐Syncope or Lightheadedness Click or tap here to enter text. ☐Headache Click or tap here to enter text. ☐Numbness Click or tap here to enter text. ☐Tingling Click or tap here to enter text. ☐Sensation Changes ☐Speech Deficits Click or tap here to enter text. ☐Other: Click or tap here to enter text.
☐Earache Click or tap here to enter text. ☐Tinnitus Click or tap here to enter text. ☐Epistaxis Click or tap here to enter text. ☐Vertigo Click or tap here to enter text. ☐Hearing Changes Click or tap here to enter text.
☐Hoarseness Click or tap here to enter text. ☐Oral Ulcers Click or tap here to enter text. ☐Sore Throat Click or tap here to enter text. ☐Congestion Click or tap here to enter text. ☐Rhinorrhea Click or tap here to enter text. ☐Other: Click or tap here to enter text.
Cardiac and Peripheral Vascular If patient denies all symptoms for this system, check here: ☐
☒Chest pain In the last month, center chest, several minutes, 5/10 pain ☐SOB Click or tap here to enter text. ☒Exercise Intolerance Pain occurred with yard work/stairs ☐Orthopnea Denies ☐Edema Denies ☐Murmurs Denies
☐Palpitations Denies ☐Faintness Denies ☐Claudications Denies ☐PND Denies ☐Other: Click or tap here to enter text.
MSK If patient denies all symptoms for this system, check here: ☐
GI If patient denies all symptoms for this system, check here: ☐
GU If patient denies all symptoms for this system, check here: ☐
PSYCH If patient denies all symptoms for this system, check here: ☐
☐Pain Click or tap here to enter text. ☐Stiffness Click or tap here to enter text. ☐Crepitus Click or tap here to enter text. ☐Swelling Click or tap here to enter text. ☐Limited ROM
☐Nausea/Vomiting Denies ☐Dysphasia Denies ☐Diarrhea Denies ☐Appetite Change Denies ☐Heartburn Denies ☐Blood in Stool Denies ☐Abdominal Pain Click or tap here to enter text. Denies ☒Food Intolerance Chest pain with big meals/steak ☐Rectal Bleeding Denies ☐Other:
☐Urgency Click or tap here to enter text. ☐Dysuria Click or tap here to enter text. ☐Burning Click or tap here to enter text. ☐Hematuria Click or tap here to enter text. ☐Polyuria Denies ☐Nocturia Denies ☐Incontinence Click or tap here to enter text. ☐Other: Click or tap here to enter text.
☐Stress Click or tap here to enter text. ☐Anxiety Click or tap here to enter text. ☐Depression Click or tap here to enter text. ☐Suicidal/Homicidal Ideation Click or tap here to enter text. ☐Memory Deficits Click or tap here to enter text. ☐Mood Changes Click or tap here to enter text. ☐Trouble Concentrating Click or tap here to enter text. ☐Other: Click or tap here to enter text.
☐Redness Click or tap here to enter text. ☐Misalignment Click or tap here to enter text. ☐Other: Click or tap here to enter text.
GYN If patient denies all symptoms for this system, check here: ☐ ☐Rash Click or tap here to enter text. ☐Discharge Click or tap here to enter text. ☐Itching Click or tap here to enter text. ☐Irregular Menses Click or tap here to enter text. ☐Dysmenorrhea Click or tap here to enter text. ☐Foul Odor Click or tap here to enter text. ☐Amenorrhea Click or tap here to enter text. ☐LMP: Click or tap here to enter text. ☐Contraception Click or tap here to enter text. ☐Other:Click or tap here to enter text.
Hematology/Lymphatics If patient denies all symptoms for this system, check here: ☐ ☐Anemia Click or tap here to enter text. ☐ Easy bruising/bleeding Click or tap here to enter text. ☐ Past Transfusions Click or tap here to enter text. ☐ Enlarged/Tender lymph node(s) Click or tap here to enter text. ☐ Blood or lymph disorder Click or tap here to enter text. ☐ Other Click or tap here to enter text.
Endocrine If patient denies all symptoms for this system, check here: ☐ ☐ Abnormal growth Click or tap here to enter text. ☐ Increased appetite Click or tap here to enter text. ☐ Increased thirst Click or tap here to enter text. ☐ Thyroid disorder Click or tap here to enter text. ☐ Heat/cold intolerance Click or tap here to enter text. ☐ Excessive sweating Click or tap here to enter text. ☐ Diabetes Click or tap here to enter text. ☐ Other Click or tap here to enter text.
O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and percussion. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings. Pertinent positive are the “abnormal” findings and pertinent “negative” are the expected normal findings. Separate the assessment findings accordingly and be detailed.
Body System
Positive Findings
Negative Findings
General Click or tap here to enter text.
Pleasant 58 y/o Male, A&Ox3, clear speech, in no physical distress or signs of pain currently. No tenting
Skin Unable to Assess
HEENT
Unable to Assess
Unable to Assess
Fine crackles in posterior right and left lung bases.
Respirations even and unlabored, breath sounds clear to auscultation in upper lobes and right middle lobe. Chest symmetric, no visible abnormalities.
Right side carotid bruit. S3 noted in mitral area.
No JVD present, JVP 3cm above sternal angle. No bruit present in left carotid. Brachial, radial, femoral pulses 2+ without thrill. Popliteal, tibial, dorsalis pedis 1+ without thrill. Cap refill...
Similar Free PDFs

NR 509 SOAP Note Week 4
- 10 Pages

NR 509 Week 1 Tina Jones SOAP note
- 12 Pages

NR 509 SOAP - B.F. Chest Pain
- 12 Pages

SOAP Wk 4 - SOAP Note
- 4 Pages

WEEK 4 SOAP NOTE Annual physical
- 6 Pages

Asthma SOAP Note - soap note
- 5 Pages

Soap Note- Abdominal - SOAP Note
- 7 Pages

Soap Note 1 - Soap
- 6 Pages

SOAP#10 - Completed SOAP note
- 1 Pages

Heent soap example - Soap note
- 2 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu





