Nursing Care Plans for Vascular Disorders PDF
| Title | Nursing Care Plans for Vascular Disorders |
|---|---|
| Author | Megan Hill |
| Course | Concepts of Chronic Care |
| Institution | Texas Tech University Health Sciences Center |
| Pages | 6 |
| File Size | 175 KB |
| File Type | |
| Total Views | 153 |
Summary
Vascular disorders -nursing care plans and interventions...
Description
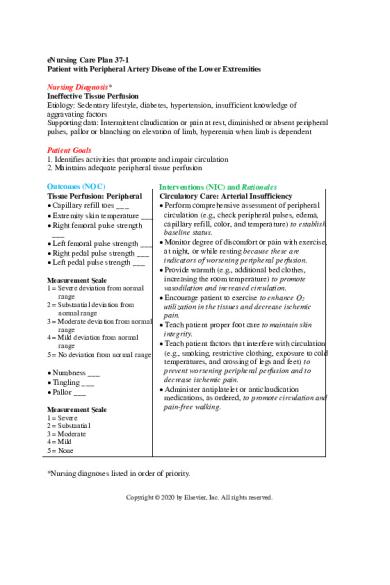
eNursing Care Plan 37-1 Patient with Peripheral Artery Disease of the Lower Extremities Nursing Diagnosis* Ineffective Tissue Perfusion Etiology: Sedentary lifestyle, diabetes, hypertension, insufficient knowledge of aggravating factors Supporting data: Intermittent claudication or pain at rest, diminished or absent peripheral pulses, pallor or blanching on elevation of limb, hyperemia when limb is dependent Patient Goals 1. Identifies activities that promote and impair circulation 2. Maintains adequate peripheral tissue perfusion Outcomes (NOC) Tissue Perfusion: Peripheral Capillary refill toes ___ Extremity skin temperature ___ Right femoral pulse strength ___ Left femoral pulse strength ___ Right pedal pulse strength ___ Left pedal pulse strength ___
Interventions (NIC) and Rationales Circulatory Care: Arterial Insufficiency Perform comprehensive assessment of peripheral circulation (e.g., check peripheral pulses, edema, capillary refill, color, and temperature) to establish baseline status. Monitor degree of discomfort or pain with exercise, at night, or while resting because these are indicators of worsening peripheral perfusion. Provide warmth (e.g., additional bed clothes, increasing the room temperature) to promote Measurement Scale vasodilation and increased circulation. 1 = Severe deviation from normal range Encourage patient to exercise to enhance O2 2 = Substantial deviation from utilization in the tissues and decrease ischemic normal range pain. 3 = Moderate deviation from normal Teach patient proper foot care to maintain skin range integrity. 4 = Mild deviation from normal Teach patient factors that interfere with circulation range (e.g., smoking, restrictive clothing, exposure to cold 5 = No deviation from normal range temperatures, and crossing of legs and feet) to prevent worsening peripheral perfusion and to Numbness ___ decrease ischemic pain. Tingling ___ Administer antiplatelet or anticlaudication Pallor ___ medications, as ordered, to promote circulation and pain-free walking. Measurement Scale 1 = Severe 2 = Substantial 3 = Moderate 4 = Mild 5 = None
*Nursing diagnoses listed in order of priority. Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan
37-2
Nursing Diagnosis Activity Intolerance Etiology: Imbalance between O2 supply and demand Supporting data: Intermittent claudication Patient Goals 1. Describes plans for a walking program 2. Has increased activity tolerance Outcomes (NOC) Activity Tolerance Walking pace ___ Walking distance ___ Ease of performing ADLs ___ Measurement Scale 1 = Severely compromised 2 = Substantially compromised 3 = Moderately compromised 4 = Mildly compromised 5 = Not compromised
Interventions (NIC) and Rationales Exercise Promotion Determine patient’s motivation to begin/continue exercise program to plan interventions. Teach patient about appropriate type of exercise for level of health, in collaboration with HCP and/or exercise physiologist, to meet needs and to prevent injury during exercise. Teach patient about desired frequency, duration, and intensity of the exercise program so endurance can be increased and O2utilization in the tissues enhanced. Teach patient proper warm-up and cool-down exercises to avoid injury.
Nursing Diagnosis Lack of Knowledge Etiology: Lack of knowledge of disease and self-care measures Supporting data: Questions about disease process, wound, and treatment Patient Goal States key elements of the therapeutic regimen, including knowledge of disease, treatment plan, reduction of risk factors, and proper ulcer/foot care Outcomes (NOC) Knowledge: Treatment Regimen Specific disease process ___ Self-care responsibilities for ongoing treatment ___ Prescribed exercise ___ Prescribed procedure ___ Benefits of disease management ___ Measurement Scale
Interventions (NIC) and Rationales Teaching: Individual Determine the patient’s ability to learn specific information (i.e., developmental level, physiologic status, orientation, pain, fatigue, unfulfilled basic needs, emotional state, and adaptation to illness) so that teaching plan can be individualized. Teaching: Disease Process Assess patient’s and caregiver’s current level of knowledge of disease related to specific disease process to determine extent of problem and plan
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan
37-3 Interventions (NIC) and Rationales appropriate intervention. Describe disease process to facilitate patient’s and caregiver’s understanding of illness. Describe common signs and symptoms of the disease so patient and caregiver can better manage illness. Discuss therapy/treatment options so patient and caregiver will be less anxious, be more cooperative with treatment plan, and make accurate adjustments in lifestyle. Discuss lifestyle changes that may be required to prevent future complications and/or control the disease process (e.g., smoking cessation, foot care) so patient can modify risk factors related to peripheral artery disease.
Outcomes (NOC) 1 = No knowledge 2 = Limited knowledge 3 = Moderate knowledge 4 = Substantial knowledge 5 = Extensive knowledge
Nursing Diagnosis Impaired Tissue Integrity Related factors: Decreased peripheral circulation, altered sensation, increased susceptibility to infection Supporting date: Damaged or destroyed tissue on lower extremities Patient Goal Maintains intact skin on lower extremities, free of infection Outcomes (NOC) Tissue Integrity: Skin and Mucous Membranes Skin temperature ___ Sensation ___ Tissue perfusion ___ Skin integrity ___ Measurement Scale 1 = Severely compromised 2 = Substantially compromised 3 = Moderately compromised 4 = Mildly compromised 5 = Not compromised
Interventions (NIC) and Rationales Circulatory Precautions Teach patient and caregiver protection from injury of affected area because tissue is very fragile and wounds heal poorly because of poor circulation. Teach patient to test bath water before entering to avoid burning skin because sensation may be diminished. Teach patient foot and nail care to avoid injury and infection of the extremity. Maintain adequate hydration to prevent increased blood viscosity. Monitor extremities for areas of heat, redness, pain, or swelling to detect infection. Skin Care: Topical Treatments Apply emollients to affected area to keep skin moist and avoid cracking.
ADLs, Activities of daily living.
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan
37-4
eNursing Care Plan 37-2 Patient after Surgical Repair of the Aorta Nursing Diagnosis* Impaired Peripheral Neurovascular Function Related factors: Graft thrombosis, embolism, prolonged aortic cross-clamping, hypotension, and/or blood loss Supporting data: Decreased or absent peripheral pulses, delayed capillary refill time, cool skin, paresthesia, edema, pain, pallor Patient Goal Maintains effective peripheral tissue perfusion Outcomes (NOC) Tissue Perfusion: Peripheral Capillary refill (toes) ___ Extremity skin temperature ___ Femoral pulse strength (right) ___ Femoral pulse strength (left) ___ Pedal pulse strength (right) ___ Pedal pulse strength (left) ___ Mean blood pressure ___ Measurement Scale 1 = Severe deviation from normal range 2 = Substantial deviation from normal range 3 = Moderate deviation from normal range 4 = Mild deviation from normal range 5 = No deviation from normal range
Muscle weakness ___ Localized extremity pain ___ Numbness ___ Tingling ___ Pallor ___
Interventions (NIC) and Rationales Circulatory Care: Arterial Insufficiency Perform a comprehensive assessment of peripheral circulation (e.g., check peripheral pulses, edema, capillary refill, color, and temperature of extremities) to establish baseline status and detect altered peripheral perfusion. Maintain adequate hydration to decrease blood viscosity. Avoid applying direct heat to the extremity because burns can occur if numbness is present. Administer antiplatelet or anticoagulant medications as appropriate to prevent thrombus formation. Neurologic Monitoring Monitor vital signs (temperature, blood pressure, pulse, respirations) for changes in neurovascular status. Monitor invasive hemodynamic parameters to identify changes from baseline. Monitor for paresthesia (numbness, tingling) as a sign of neurologic impairment.
Measurement Scale
*Nursing diagnoses listed in order of priority. Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan
37-5 Interventions (NIC) and Rationales
Outcomes (NOC) 1 = Severe 2 = Substantial 3 = Moderate 4 = Mild 5 = None
Nursing Diagnosis Impaired Urinary System Function Risk factors: Graft thrombosis, embolism, hemorrhage, and/or prolonged aortic crossclamping Supporting data: Anuria, oliguria, high blood urea nitrogen (BUN)/creatinine Patient Goal Maintains effective renal perfusion Outcomes (NOC) Tissue Perfusion: Abdominal Organs Mean blood pressure ___ Urine output ___ Urine specific gravity ___ Blood urea nitrogen ___ Plasma creatinine ___ Electrolyte and acid-base balance ___ Measurement Scale 1 = Severe deviation from normal range 2 = Substantial deviation from normal range 3 = Moderate deviation from normal range 4 = Mild deviation from normal range 5 = No deviation from normal range
Interventions (NIC) and Rationales Hemodynamic Regulation Monitor intake/output, urine output, and patient weight to detect signs of altered renal perfusion. Monitor electrolyte levels to detect altered renal function. Maintain fluid balance by administering IV fluids to ensure adequate hydration and renal perfusion. Evaluate effects of fluid therapy to ensure adequate hydration. Administer vasodilator and/or vasoconstrictor medication, as appropriate, to maintain adequate renal artery perfusion.
Nursing Diagnosis Risk for Infection Risk factors: multiple invasive lines/tubes, surgical incision, and presence of a prosthetic vascular graft Patient Goal Has no infection Outcomes (NOC)
Interventions (NIC) and Rationales
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan
37-6
Interventions (NIC) and Rationales Outcomes (NOC) Infection Severity Infection Protection Fever ___ Monitor for systemic and localized signs and Wound site culture colonization symptoms of infection (e.g., elevated body temperature, heart rate, respiratory rate, decreased ___ blood pressure, erythema and warmth along the White blood count elevation incision line, purulent drainage from incision) to ___ establish baseline and detect changes in status. Purulent drainage ___ Monitor absolute granulocyte count, WBC count, and differential results because increasing counts Measurement Scale 1 = Severe may indicate infection. 2 = Substantial Maintain asepsis for patient at risk because incision 3 = Moderate sites and indwelling lines are potential portals for 4 = Mild infection. 5 = None Teach patient to take antibiotics as prescribed to maintain adequate blood levels of the drug. Wound Healing: Primary Promote sufficient nutritional intake to promote Intention healing. Serosanguineous drainage ___ Sanguineous drainage ___ Periwound edema ___ Increased skin temperature ___ Surrounding skin erythema ___ Measurement Scale 1 = Extensive 2 = Substantial 3 = Moderate 4 = Limited 5 = None
Copyright © 2020 by Elsevier, Inc. All rights reserved....
Similar Free PDFs

Anemia Nursing Care Plans
- 7 Pages

Vascular- Disorders
- 3 Pages

Nursing care plans hypovolemic shock
- 14 Pages

Chapter 37 Vascular Disorders
- 16 Pages

Care plan for nursing
- 1 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu










