8 13 December 2018, questions and answers PDF
| Title | 8 13 December 2018, questions and answers |
|---|---|
| Course | Pathology & Therapeutics I |
| Institution | George Brown College |
| Pages | 15 |
| File Size | 298.9 KB |
| File Type | |
| Total Downloads | 13 |
| Total Views | 163 |
Summary
Test questions and answers with rationale ...
Description
A) B) C) D) Ans:
A) B) C) D) Ans:
A) B) C) D) Ans:
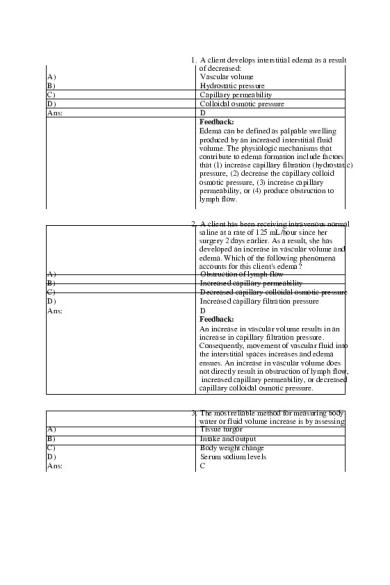
1. A client develops interstitial edema as a result of decreased: Vascular volume Hydrostatic pressure Capillary permeability Colloidal osmotic pressure D Feedback: Edema can be defined as palpable swelling produced by an increased interstitial fluid volume. The physiologic mechanisms that contribute to edema formation include factors that (1) increase capillary filtration (hydrostatic) pressure, (2) decrease the capillary colloid osmotic pressure, (3) increase capillary permeability, or (4) produce obstruction to lymph flow. 2. A client has been receiving intravenous normal saline at a rate of 125 mL/hour since her surgery 2 days earlier. As a result, she has developed an increase in vascular volume and edema. Which of the following phenomena accounts for this client's edema? Obstruction of lymph flow Increased capillary permeability Decreased capillary colloidal osmotic pressure Increased capillary filtration pressure D Feedback: An increase in vascular volume results in an increase in capillary filtration pressure. Consequently, movement of vascular fluid into the interstitial spaces increases and edema ensues. An increase in vascular volume does not directly result in obstruction of lymph flow, increased capillary permeability, or decreased capillary colloidal osmotic pressure. 3. The most reliable method for measuring body water or fluid volume increase is by assessing: Tissue turgor Intake and output Body weight change Serum sodium levels C
Feedback: Daily weights are a reliable index of water volume gain (1 L of water weighs 2.2 pounds). Daily weight measurements taken at the same time each day with the same amount of clothing provide a useful index of water gain due to edema. When an unbalanced distribution of body water exists in the tissues and organs, assessment of surface skin tissue tur gor will be inaccurate. Measurement of renal ou tput is unreliable because fluid retention may be a compensatory response, or the renal system may be dysfunctional. Serum sodium levels are affected by multiple variables other than body water volume.
A) B) C) D) Ans:
4. A client with a diagnosis of liver cirrhosis secondary to alcohol abuse has a distended abdomen as a result of fluid accumulation in his peritoneal cavity (ascites). Which of the following pathophysiologic processes contributes to this third spacing? Abnormal increase in transcellular fluid volume Increased capillary colloidal osmotic pressure Polydipsia Impaired hormonal control of fluid volume A Feedback: Third spacing represents the loss or trapping of extracellular fluid (ECF) in the transcellular spa ce and a consequent increase in transcellular flu id volume. The serous cavities are part of the tra nscellular compartment located in strategic body areas where there is continual movement of body structures—the pericardial sac, the peri toneal cavity, and the pleural cavity. Polydipsia and increased fluid intake alone are insufficient to cause third spacing, and increased capillary colloidal osmotic pressure would result in increased intracellular fluid (ICF ). The etiology of third spacing does not normally include alterations in hormonal control of fluid balance.
A) B) C) D) Ans:
A) B) C) D) Ans:
5. A 2-week-old infant (full-term at birth) is admitted to the pediatrics unit with “spitting up large amounts of formula” and diarrhea. The infant has developed a weak suck reflex. Which of the following statements about total body water (TBW) is accurate in this situation? About 52% of the infants' weight accounts for the amount of water in their body. Because of the infants' higher fat ratio, one should anticipate an increased TBW to as high as 90%. Most full-term infants have a TBW of approximately 75% due to their high metabolic rate. Most of an infant's TBW remains in the ICF com partment, so they should be able to transfer needed water into the ECF space. C Feedback: Infants normally have more TBW than older children or adults. TBW constitutes approximately 75% to 80% of body weight in full-term infants and an even greater percentage in premature infants. In males, the TBW decrea ses in the elderly population to approximately 52% TBW. Obesity decreases TBW, with levels as low as 30% to 40% of body weight in adults. Infants have more than half of their TBW in their ECF compartment, as compared to adults. 6. A client diagnosed with schizophrenia has been admitted to the emergency department (ED) after ingesting more than 2 gallons of water in one sitting. Which of the following path ophysiologic processes may result from the sudden water gain? Hypernatremia Water movement from the extracellular to the in tracellular compartment Syndrome of inappropriate secretion of ADH (S IADH) Isotonic fluid excess in the extracellular fluid compartment B Feedback: Excess water ingestion coupled with impaired water excretion (or rapid ingestion at a rate
that exceeds renal excretion) in persons with psychogenic polydipsia can lead to water intoxication (hyponatremia). A disproportionate gain of water with no accompanying gain in sodium results in the movement of water from the extracellular to the intracellular compartment. Hyponatremia ac companies this process. Because of the lack of sodium increase, accumulated fluid is hypotonic , not isotonic. SIADH is not a consequence of excess water intake.
A) B) C) D) Ans:
A) B) C) D) Ans:
7. A nurse caring for a client with a diagnosis of diabetes insipidus (DI) should prioritize the close monitoring of which of the following electrolyte levels? Potassium Sodium Magnesium Calcium B Feedback: The high water intake and high urine output that characterize diabetes insipidus create a risk of sodium imbalance. DI may present with hype rnatremia and dehydration, especially in persons without free access to water, or with damage to the hypothalamic thirst center and altered thirst sensation. 8. The syndrome of inappropriate antidiuretic hormone (SIADH) is characterized by: Increased osmolality level of 360 mOsm/kg Excessive thirst with fluid intake of 7000 mL/da y Copious dilute urination with output of 5000 mL /day Low serum sodium level of 122 mEq/L D Feedback: SIADH results from a failure of the negative feedback system that regulates the release and inhibition of antidiuretic hormone (ADH). ADH secretion continues even when serum osmolalit
y is decreased, causing water retention and dilut ional hyponatremia. Diabetes insipidus, deficiency or decreased response to ADH, is characterized by increased serum osmolality, excessive thirst, and polyuria. Urine output decreases in SIADH despite adequate or increased fluid intake.
A) B) C) D) Ans:
A) B) C) D) E) Ans:
9. In isotonic fluid volume deficit, changes in total body water are accompanied by: Intravascular hypotonicity Increased intravascular water Increases in intracellular sodium Proportionate losses of sodium D Feedback: Isotonic fluid volume deficit causes a proportionate loss of sodium and water. Hypoto nicity results from water retention or sodium loss. Increased intravascular water causes sodium to move into the cell excessively. 10. A client with a history of heart and kidney failure is brought to the emergency department. Upon assessment/diagnosis, it is determined the client is in decompensated heart failure. Of the following assessment findings, which are associated with excess intracellular water? Select all that apply. Lethargy Confusion Hyperactive deep tendon reflexes Seizures Firm, rubbery tissue when palpating lower extremities A, B, D Feedback: Hyponatremia is usually defined as a serum sodium concentration of less than 135 mEq/L. Muscle cramps, weakness, and fatigue reflect the effects of hyponatremia on skeletal muscle function and are often early signs of hyponatrem
ia. The cells of the brain and nervous system are the most seriously affected by increases in intracellular water. Symptoms include apathy, lethargy, and headache, which can progress to disorientation, confusion, gross motor weakness, and depression of deep tendon reflexes. Seizures and coma occur when serum sodium levels reach extremely low levels. Hypovolemia, third spacing (maldistribution of body fluid), and dehydration are associated with hypernatremia and/or hypertonicity.
A) B) C) D) Ans:
11. Which of the following assessments should be prioritized in the care of a client who is being treated for a serum potassium level of 2.7 mEq/ L? Detailed fluid balance monitoring checking for pitting edema Arterial blood gases looking for respiratory alka losis Cardiac monitoring looking for prolonged PR interval and flattening of the T wave Monitoring of hemoglobin levels and oxygen saturation C Feedback: The most serious effects of hypokalemia are on the heart, a fact that necessitates frequent ele ctrocardiography or cardiac telemetry. Hypokale mia produces a decrease in the resting membrane potential, causing prolongation of the PR interval. It also prolongs the rate of ventricular repolarization, causing depression of the ST segment, flattening of the T wave, and appearance of a prominent U wave. This supersedes the importance of fluid balance monitoring, arterial blood gases, oxygen saturation, or hemoglobin levels.
A) B) C) D) Ans:
A) B) C) D) E) Ans:
12. Of the following clients, which would be at highest risk for developing hyperkalemia? A male admitted for acute renal failure following a drug overdose A client diagnosed with an ischemic stroke with multiple sensory and motor deficits An elderly client experiencing severe vomiting and diarrhea as a result of influenza A postsurgical client whose thyroidectomy resulted in the loss of some of the parathyroid g lands A Feedback: There are three main causes of hyperkalemia: (1) decreased renal elimination; (2) a shift in potassium from the ICF to ECF compartment; and (3) excessively rapid rate of administration. The most common cause of serum potassium excess is decreased renal function. Stroke does not typically have a direct influence on potassium levels, whereas vomiting and diarrhea can precipitate hypokalemia. Loss of the parathyroid influences calcium, not potassium, levels. 13. A heart failure client has gotten confused and took too many of his “water pills” (diuretics). On admission, his serum potassium level was 2.6 mEq/L. Of the following assessments, which correlate to this hypokalemia finding? Select all that apply. Polyuria Constipation Bradycardia Paresthesia with numbness of the lips/mouth ECG showing short runs of ventricular fibrillati on A, B, D Feedback: The manifestations of hypokalemia include alterations in neuromuscular, gastrointestinal, re nal, and cardiovascular function. There are numerous signs and symptoms associated with g astrointestinal function, including anorexia, nausea, and vomiting. Atony of the gastrointesti nal smooth muscle can cause constipation, abdominal distention, and, in severe hypokalem
ia, paralytic ileus. Urine output and plasma osm olality are increased; urine specific gravity is decreased; and complaints of polyuria, nocturia, and thirst are common. The most serious effects of hypokalemia are on the heart. The first symptom associated with hyperkalemia typically is paresthesia (a feeling of numbness and tingling). Hyperkalemia results in prolongation of the PR interval; widening of the QRS complex with no change in its configuration; and decreased amplitude, widening, and eventual disappearance of the P wave. The heart rate may be slow. Ventricular fibrillation and cardiac arrest are terminal events.
A) B) C) D) Ans:
14. A client has been admitted for deterioration of her renal function due to chronic renal failure. Her admission K + level is 7.8 mEq/L. The nurse would expect to see which of the following abnormalities on her telemetry (ECG) strip? Select all that apply. Tachycardia (fast rate) with frequent early ventricular beats (PVCs) Prolonged PR interval with widening of the QR S complex Ventricular fibrillation Atrial flutter with a 2:1 conduction ratio B, C Feedback: Hyperkalemia decreases membrane excitability, producing a delay in atrial and ventricular depolarization, and it increases the rate of ventricular repolarization. If serum K+ levels continue to rise (above 6 mEq/L), there is a prolongation of the PR interval; widening of the QRS complex with no change in its configuration; and decreased amplitude and widening and eventual disappearance of the P
wave. The heart rate may be slow. Ventricular f ibrillation and cardiac arrest are terminal events
A) B) C) D) Ans:
A) B) C)
15. Hypoparathyroidism causes hypocalcemia by: Increasing serum magnesium Increasing phosphate excretion Blocking release of calcium from bone Blocking action of intestinal vitamin D C Feedback: The most common causes of hypocalcemia are abnormal losses of calcium by the kidney, impaired ability to mobilize calcium from bone due to hypoparathyroidism, and increased protein binding or chelation such that greater proportions of calcium are in the no nionized form. Magnesium deficiency inhibits P TH release and impairs PTH action on bone reso rption. Phosphate and calcium are inversely related, and PTH does not control phosphate ex cretion. PTH does not exert control of vitamin D action in the intestine, but elevated vitamin D levels can suppress PTH release. 16. A female client with a history of chronic renal fa ilure has a total serum calcium level of 7.9 mg/d L. While performing an assessment, the nurse should focus on which of the following clinical manifestations associated with this calcium level? Complaints of shortness of breath on exertion with decreased oxygen saturation levels Difficulty arousing the client and noticing she is disoriented to time and place Heart rate of 120 beats/minute associated with d iaphoresis (sweaty)
D) Ans:
A) B) C) D) E) Ans:
Intermittent muscle spasms and complaints of numbness around her mouth D Feedback: Spasms and numbness are characteristic of hypo calcemia. Respiratory effects, tachycardia, and d iaphoresis are not associated with low calcium levels, whereas decreased level of consciousness can be indicative of hypercalcem ia. 17. An elderly client is admitted with elevated magnesium level related to a history of renal ins ufficiency and excess use of antacids and laxatives containing magnesium. On admission assessment, the nurse notes which clinical manifestations that correlate to hypermagnesem ia? Select all that apply. Hyporeflexia Blood pressure 180/90 Tetanic muscle contractions Muscle weakness causing shallow breathing Paresthesia of the lips A, D Feedback: The signs and symptoms occur only when serum magnesium levels exceed 4.0 mg/dL. Hy permagnesemia affects neuromuscular and cardiovascular function. Increased levels of magnesium cause hyporeflexia and muscle weakness. Blood pressure is decreased, and the ECG shows an increase in the PR interval, a shortening of the QT interval, T-wave abnormalities, and prolongation of the QRS and PR intervals. Severe hypermagnesemia is associated with muscle and respiratory paralysis, complete heart block, and cardiac arrest. Signs of magnesium deficiency are not usually apparent until the serum magnesium is less than 1.0 mEq/L. Hypomagnesemia is characterized by an increase in neuromuscular excitability as evidenced by hyperactive deep tendon reflexes, paresthesias (i.e., numbness, pricking, tingling sensation), muscle fasciculations, and tetanic muscle contractions.
A) B) C) D) Ans:
A) B) C) D) Ans:
18. Magnesium is important for the overall function of the body because of its direct role in: Cell membrane permeability Somatic cell growth control Sodium and tonicity regulation DNA replication and transcription D Feedback: Magnesium is essential to all reactions that require ATP, for every step related to replication and transcription of DNA, and for translation of messenger RNA. Magnesium does not have a direct role in controlling the growth of cells, extracellular tonicity and sodium balance, or permeability of the cell surface. 19. Which of the following scenarios place the client at a high risk for developing hypoparathyr oidism and require close supervision for assessing for development of muscle cramps, ca rpopedal spasm, convulsions, and paresthesia in the hands and feet? Select all that apply. A neck cancer client returning from OR after having a radical neck dissection A hyperthyroid client experiencing a “thyroid storm” requiring urgent thyroidectomy A client with seizure experiencing some anoxic deficits and memory loss A client with a history of human papillomavirus (HPV) in the uvula A, B Feedback: Hypoparathyroidism reflects deficient PTH secr etion, resulting in low serum levels of ionized c alcium. PTH deficiency may occur because of a congenital absence of all of the parathyroid gl ands or because of an acquired disorder due to inadvertent removal or irreversible damage to the glands during thyroidectomy, parathyroidect omy, or radical neck dissection for cancer. Seizures or history of HPV is not associated with this disorder.
A) B) C) D) Ans:
A) B) C) D) Ans:
20. As other mechanisms prepare to respond to a pH imbalance, immediate buffering is a result of increased: Intracellular albumin Hydrogen/potassium binding Sodium/phosphate anion absorption Bicarbonate/carbonic acid regulation D Feedback: The bicarbonate buffering system, which is the principal ECF buffer, uses H 2 CO 3 as its weak acid and bicarbonate salt such as sodium bicarbo nate (NaHCO 3 ) as its weak base. It substitutes the weak H 2 CO 3 for a strong acid such as hydro chloric acid or the weak bicarbonate base for a strong base such as sodium hydroxide. The bica rbonate buffering system is a particularly efficient system because its components can be readily added or removed from the body. Hydrogen and potassium exchange freely across the cell membrane to regulate acid–base balance. Sodium is not part of the buffering system. Intracellular protein is part of the body protein buffer system; albumin is extracellular. 21. Arterial blood gases of a client with a diagnosis of acute renal failure reveal a pH of 7.25, HCO 3 – level of 21 mEq/L, and decreased PCO 2 level accompanied by a respiratory rate of 32. This client is most likely experiencing which disorder of acid–base balance? Metabolic acidosis Metabolic alkalosis Respiratory acidosis Respiratory alkalosis A Feedback: Metabolic acidosis involves a decreased serum H CO 3 – concentration along with a decrease in pH In metabolic acidosis, the body compensates for the decrease in pH by increasing the respiratory rate in an effort to decrease PCO 2 an d H 2 CO 3 levels.
A) B) C) D) Ans:
22. A client is brought to the emergency department semicomatose and a blood glucose reading of 673. He is diagnosed with diabetic ke toacidosis (DKA). Blood gas results are as follows: serum pH 7.29 and HCO 3 – level 19 mE q/dL; PCO 2 level 32 mm Hg. The nurse should anticipate that which of the following orders may correct this diabetic ketosis? Administration of potassium chloride Initiating an insulin IV infusion along with fluid replacement Administering supplemental oxygen and rebreat hing from a paper bag Instituting a cough and deep breathing schedule for every hour while awake to improve ventilation B Feedback: The treatment of metabolic acidosis focuses on correcting the condition that is causing the disorder and restoring the fluids and electrolytes that have been lost from the body. For example, insulin administration and fluid replacement are frequently sufficient to correct a low pH in persons with diabetic ketosis. Administration of potassium chloride is used as a treatment of metabolic alkalosis. Administering supplemental oxygen and rebreathing from a paper bag are usual treatment of respiratory alkalosis. Instituting a cough and deep breathing schedule for every hour while awake to im...
Similar Free PDFs

Exam 13 May 2018, questions and answers
- 145 Pages

Final December 2018, questions
- 7 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu













