BMS2032M Clinical Biochem TCA Mock paper with answers PDF

| Title | BMS2032M Clinical Biochem TCA Mock paper with answers |
|---|---|
| Course | Clinical Biochemistry & Diagnostics |
| Institution | University of Lincoln |
| Pages | 8 |
| File Size | 290.1 KB |
| File Type | |
| Total Downloads | 102 |
| Total Views | 161 |
Summary
With answers from Carol's workshop...
Description
College of Science School of Life Sciences Time Constrained Assessment Department Module Title Module Code Module Coordinator Duration of Assessment Date Release Time Submission Time (normal) Submission Time (LSP) Word limit (if required) Is Referencing Required
School of Life Sciences Clinical Biochemistry & Diagnostics BMS2032M Carol Rea 3 Hours TBC August 15:00 18:00 19:00 2000 words maximum No
General Instructions to Candidates. 1. You must submit your answers as a MS Word Document to Turnitin on Blackboard before the submission time: failure to do so will be classified as misconduct in examinations and your work will NOT be marked. We strongly recommend you submit 15 minutes prior to the deadline. 2. You must also send a copy of your work to the email address [email protected] at the same time. Please place the Module Code and your Student ID in the Subject Field of the Mail. This must also be before the deadline of the assessment and be sent from your UNIVERSITY e-mail account. 3. If you are submitting hand-written notes or diagrams, these must be photographed (preferably using Microsoft Lens which is available as part of your Office 365 package) and inserted into the Word Document as an image. 4. This assessment is an open resource format: you may use online resources, lecture and seminar notes, text books and journals. 5. All work will be subject to plagiarism and academic integrity checks. In submitting your assessment you are claiming that it is your own original work; if standard checks suggest otherwise, Academic Misconduct Regulations will be applied. 6. The duration of the Time Constrained Assessment will vary for those students with LSPs. Extensions do not apply, but Extenuating Circumstances can be applied for in the normal way.
Module Specific Instructions to Candidates You are able to submit multiple times to blackboard, but each successive file will overwrite the previous upload. Students are advised to upload periodically throughout the TCA so that if you miss the deadline, we will still have the most recently uploaded file to mark. You must also send a copy of your work to the email address [email protected] at the same time. Please place the Module Code and your Student ID in the Subject Field of the Mail.
Please answer Clinical Problem 1 (choose only either part A or B), Clinical Problem 2 and Clinical Problem 3 Maximum total word limit of 2000 words across the whole answer.
Please answer Clinical Problem 1 (choose only either part A or B), Clinical Problem 2 and Clinical Problem 3 Maximum total word limit of 2000 words across the whole answer. Clinical Problem 1 (choose only either part A or B) A. A 37 year old man comes into the doctors complaining of abdominal pain and chronic diarrhoea. He reports that he has been feeling nauseous and vomiting within the last few weeks, and has also noticed that his clothes have suddenly become quite loose. The patient also reports that he has been struggling to concentrate at work as has been feeling tired all the time. He has some general aching and weirdly seems to be itching more than normal. The doctor has suggested that the patient might have coeliac disease. a) Based on the information above, describe how the doctor came to his diagnosis? (15 marks) He is within the main age range for people who go on to develop CD although more commonly seen in females not males (2 mark) Chronic diarrhoea (one of 4 main systems) and abdominal pain (additional symptom) are both signs of CD (2 marks) Clothes becoming lose suggests some form of weight loss and with other symptoms suggests some form of malabsorption (1 marks) and could also have bloating and excessive fat secretion (although not obvious from the current clinical info) as would be the four main symptoms (2 marks) Tiredness could be linked to malabsorption (main feature) or could be due to something else which can co-cluster such as sub-clinical iron deficiency or aneamia (2 mark) also aches could be due to osteoporosis but unlikely due to age of patient (1 mark) Itching could suggest Dermatitis Herpetiformis - features small groups of blisters, often on red plaques, situated on the back of elbows & forearms, buttocks & front of knees – these then burst causing itching (3 marks) Whilst very rare (only seen in 1 in 15000 patients) is more common in males and he is in age group for this 15-40 (2 marks)
b) The doctor also asks the patient whether they have a family history of endocrine disease. Why did the doctor ask this? (10 Marks) CD is increased with those with first degree relative with type 1 diabetes, autoimmune thyroid disease or other autoimmune disease (2 marks)
NICE guidelines for treatment specifically state that children & adults with autoimmune thyroid disease, type 1 diabetes should be screened for CD (2 marks) HLA-DQ2 haplotype (DQA1*0501/DQB1*0201) is expressed in the majority of patients with CD (90%). Most of the remaining patients carry the HLA-DQ8 haplotype (DQA1*0301/DQB1*0302). Type 1 diabetes is associated with the same DQ molecules & shares other genetics factors that contribute to both diseases (4 marks) Also key to remember these are just co-clustering of disease as can also not have any other autoimmune diseases or these may not have shown up or been tested for (AITD) tends to affect people at an older age although T1D would be more obvious (2 marks)
B. A 4 year old intact male dog was taken to the vet because of intermittent weakness and lameness. Upon examination he was found to be mildly dehydrated, with foul smelling breath and teeth covered in tartar. He had a history of longstanding standing polydipsia. Serum Biochemistry Blood urea nitrogen 65.3 mmol/L (RR 2.5-10) Creatinine 716 µmol/L (RR 79-150) Ca2+ 2.05 mmol/L (RR 2.25-2.8) Phosphate 5.5 mmol/L (RR 0.9-2.9) • Glucose, total protein, albumin, globulin, total bilirubin, cholesterol, ALT, AST, ALP, Na+, K+, Cl-, TCO2, Anion gap all within reference range Full blood count revealed a normocytic anaemia with a low red cell count Urinalysis Specific gravity suggests inability to concentrate urine. Leukocyte numbers suggest inflammation in urinary tract a. Discuss the test results (20 marks) Urea and creatinine are high (2 marks) Both indicate impaired GFR, creatinine can be used to estimate GFR (3 marks) Calcium is low (1 mark) Common in CRF (1 mark) May explain weakness and lameness as affects muscle and bone (4 marks) Normal glucose rules out DM as cause of polydipsia (2 marks) Normal TCO2 and anion gap – no metabolic acidosis (2 marks) Low red cell count due to lack of erythropoietin from kidney (2 marks) Phosphate is high (1 mark) Tends to mirror calcium, due to low GFR (2 marks) b. What is a possible cause of the hypocalcaemia and how would you confirm this? (5 marks) May be due to increased urinary loss (1 mark) More likely due to reduced vitamin D hydroxylation in CRF (3 marks)
Measure 1,25 dihydroxy vitamin D (1 mark) Clinical Problem 2 A 48 year old woman went to see her GP as she had a felt unwell for the last 2 days, feeling nauseous and hadn’t wanted to eat, she had a fever and flu-like symptoms. She had become particularly concerned when she noticed passing dark urine. The GP examined her abdomen and found tenderness over the liver, so took blood for liver function tests and sent it to the local laboratory. Serum test Total Bilirubin Aspartate aminotransferase Alanine aminotransferase Alkaline phosphatase Albumin
Test Result 62 µmol/L 935U/L 2700 U/L 412 U/L 35 g/L
Reference range (3-22 µmol/L) (12-48 U/L) (3-55 U/L) (80-280 U/L) (35-55 g/L)
A. Comment on the results, what do they indicate about the health of her liver? (20 Marks) Bilirubin is high (1 mark), could be due to haemolysis or liver disease (2 marks) symptoms suggest latter (1 mark) AST is high, (1 mark) may be due to muscle damage e.g. MI (1 mark) or liver disease (1 mark), symptoms and other tests suggest latter (1 mark) ALT high (1 mark) most commonly due to liver disease (1 mark) ALP is high (1 mark), may be due to liver disease or bone disease (2 marks) Rises in AST/ALT higher than in biliruibin and ALP (3 marks) Indicates liver disease is likely to be hepatocellular rather than cholestatic (2 marks) Albumin is normal, but is usually normal in acute liver disease (2) B. Suggest TWO different possible causes of these changes and how they could impact upon liver health (10 Marks) Can be caused by drugs e.g. paracetamol, toxins e.g. carbon tetrachloride (5 marks) Can be caused by viral hepatitis, most likely Hep A, Hep B or Hep C, fits with flu-like symptoms and fever (5 marks) or anything reasonable
C. Suggest some further tests (laboratory or other) or information that might help to distinguish the cause. (10 Marks) Clinical history to assess possible toxicity, ask about drug use, e.g. paracetamol for fever (3) Viral hepatitis, serology to measure antibodies to Hep A, Hep B, Hep C or core antigen or PCR (up to 3) occupational history to assess risk of toxin exposure (1), ultrasound scan of liver, measurement or
direct and indirect bilirubin (3) or anything reasonable up to a maximum of 10 marks D. Summarise the key advantages of “Intelligent Liver Function Testing” (10 Marks) LFTs are commonly abnormal, the causes of which can be complex and are frequently under investigated. (3) This can lead to missed opportunities to diagnose and treat liver disease at an early stage. (2) An automated investigation algorithm, intelligent liver function testing (iLFT), aims to increase the early diagnosis of liver disease in a cost-effective manner. (3) Involves liver fibrosis estimation, and reflex testing (2) or anything else reasonable up to a maximum of 10 marks
Clinical Problem 3 You have three preparations of a coloured protein and want to determine the concentration of each by comparing with standard solutions of the protein of known concentration. Figure 1 shows the absorbance spectra of a range of concentrations of the standard protein when measured using UV/Vis spectroscopy in a cuvette of path length 1 cm. From the data below: A. Construct a graph that demonstrates the relationship of absorbance at 488 nm and protein concentration. (12 marks) B. Using this graph, calculate a line of best fit and determine the extinction coefficient of the protein at 488 nm.
(7 marks)
C. Calculate the concentrations of the unknown samples of the protein and comment on the accuracy of the values obtained. How could you reduce the error in the assay?
(6 marks)
Figure 1: Absorbance of the novel coloured protein at the indicated wavelength.
Unknown 1 has absorbance at 488 nm = 0.15 Unknown 2 has absorbance at 488 nm = 0.32 Unknown 3 has absorbance at 488 nm = 2.55 Answer ; a)
Figure 1: Correlation of protein concentration and absorbance at 488 nm for a novel coloured protein Sensible scale on each axis [2]
Each axis correctly labelled [1] with units [1] Figure number [1] and title [1] Data points accurately determined and plotted [3] Appropriate line of best fit [1] that passes through the origin [1] Neatly presented [1] Marks can be deducted for incorrect formatting such as having a title on the graph or inappropriate size of graph. b) The line of best fit should have the equation y = 0.05x [2] Gradient of the line should be calculated e.g. 1/20 = 0.05 [1] Using the equation A=ecl [1] l is equal to 1 [1] so this is equivalent to y = mx [1] so the extinction coefficient = 0.05 mM-1 cm-1 [1]
c) Using the line of best fit calculated above and rearranging: X = y/0.05 [1] Unknown 1 = 3 mM [1] (0.5 if no units)] Unknown 2 = 6.4 mM [1] (0.5 if no units)] Unknown 3 = 51 mM [1] (0.5 if no units)] Unknown 3 is unlikely to be correct as the value for the absorbance is significantly in excess of 1 [1]. This could be improved by diluting the sample prior to measurement or decreasing the path length [1]....
Similar Free PDFs

Mock exam with answers
- 10 Pages
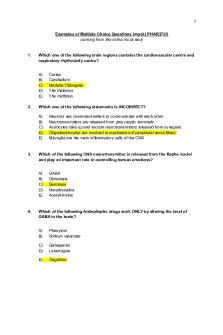
MCQs mock-PHAR3703 with Answers
- 10 Pages

FMI - Mock General answers
- 6 Pages

4PY019 IDM Mock exam paper
- 6 Pages

mock Exam 2017, answers
- 11 Pages

MOCK EXAM ANSWERS
- 24 Pages

1- Mock Exam paper 2018
- 13 Pages

Mat mock test paper 2
- 11 Pages

ISE II Sample paper 3 with answers
- 13 Pages

Mock Exam Paper 1 - ECS1500
- 19 Pages

Unit 313 Mock 2 paper
- 5 Pages

Unit 313 Mock 1 paper
- 5 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu



