Chapter 68-ppt - med surg 2 PDF

| Title | Chapter 68-ppt - med surg 2 |
|---|---|
| Course | Medical-Surgical Nursing II |
| Institution | National University (US) |
| Pages | 19 |
| File Size | 88.6 KB |
| File Type | |
| Total Downloads | 772 |
| Total Views | 926 |
Summary
Ch 68 A broad classification that includes injury to the scalp, skull, or brain 2 million people receive head injuries every year in the United States The most common cause of death from trauma Most common cause of brain trauma is falls Immediate complications include cerebral bleeding, hem...
Description
Ch 68
A broad classification that includes injury to the scalp, skull, or brain 2.5 million people receive head injuries every year in the United States The most common cause of death from trauma Most common cause of brain trauma is falls Immediate complications include cerebral bleeding, hematomas, uncontrolled increased in ICP, infections, and seizures. Groups at highest risk for brain trauma include children 0 to 4 years old, adolescents ages 15 to 19 years, and adults 65 years and older Prevention is the best approach
PATHOPHYSIOLOGY OF TRAUMATIC BRAIN INJURY
Closed brain injury (blunt trauma): acceleration/deceleration injury occurs when the head accelerates and then rapidly decelerates, damaging brain tissue Skull Fractures: linear, depressed, compound, comminuted Concussion: a temporary loss of consciousness with no apparent structural damage Contusion: bruising type of injury to the brain tissue; more severe injury with possible surface hemorrhage Symptoms and recovery depend on the amount of damage and associated cerebral edema Longer period of unconsciousness with more symptoms of neurologic deficits and changes in vital signs Diffuse axonal injury: widespread axon damage in the brain seen with head trauma. Patient develops immediate coma.
Manifestations depend on the severity and location of the injury Scalp wounds Tend to bleed heavily and are portals for infection Skull fractures Usually have localized, persistent pain Fractures of the base of the skull Bleeding from nose pharynx or ears Battle sign—ecchymosis behind the ear CSF leak: halo sign—ring of fluid around the blood stain from drainage
Patient may be admitted for observation or sent home Observation of patients after head trauma; report immediately Observe for any changes in LOC Difficulty in awakening, lethargy, dizziness, confusion, irritability, anxiety Difficulty in speaking or movement Severe headache Vomiting Patient should be aroused and assessed frequently
Open brain injury: object penetrates the brain or trauma is so severe that the scalp and skull are opened. Scalp lacerations Fractures in the skulls Interruption of the dura matter
Assume cervical spine injury until it is ruled out Therapy to preserve brain homeostasis and prevent secondary damage Treat cerebral edema Maintain cerebral perfusion; treat hypotension, hypovolemia, and bleeding; monitor and manage ICP Maintain oxygenation; cardiovascular and respiratory function Manage fluid and electrolyte balance
Primary brain injury/traumatic Open versus closed head injuries Mild, moderate, severe classification Fractures Secondary brain injury/nontraumatic Any processes that occur after the initial injury and worsen patient outcomes Damage occurs because delivery of oxygen and glucose to the brain is interrupted Examples: Intracranial Copyright © 2018 Elsevier Inc. All rights reserved. 14
Primary injury: consequence of direct contact to head/brain during the instant of initial injury Contusions, lacerations, external hematomas, skull fractures, subdural hematomas, concussion, diffuse axonal Secondary injury: damage evolves over ensuing days and hours after the initial injury Caused by cerebral edema, ischemia, or chemical changes associated with the trauma
Altered LOC Pupillary abnormalities Sudden onset of neurologic deficits and neurologic changes; changes in sense, movement, reflexes Changes in vital signs Headache Seizures
Intracranial bleeding Epidural hematoma Subdural hematoma Acute and subacute Chronic Intracerebral hemorrhage and hematoma Subarachnoid hemorrhage
Blood collection in the space between the skull and the dura Patient may have a brief loss of consciousness with return of lucid state; then as hematoma expands, increased ICP will often suddenly reduce LOC An emergency situation! Treatment includes measures to reduce ICP, remove the clot, and stop bleeding (burr holes or craniotomy) Patient will need monitoring and support of vital body functions; respiratory support
19
Copyright © 2018 Elsevier Inc. All rights reserved.
LOCATION OF SUBDURAL, INTRACEREBRAL,AND EPIDURAL HEMORRHAGES
Collection of blood between the dura and the brain Acute or subacute Acute: symptoms develop over 24 to 48 hours Subacute: symptoms develop over 48 hours to 2 weeks Requires immediate craniotomy and control of ICP Chronic Develops over weeks to months Causative injury may be minor and forgotten Clinical signs and symptoms may fluctuate
Treatment is evacuation of the clot
Hemorrhage occurs into the substance of the brain May be caused by trauma or a nontraumatic cause Treatment Supportive care Control of ICP Administration of fluids, electrolytes, and antihypertensive medications Craniotomy or craniectomy to remove clot and control hemorrhage; this may not be possible because of the location or lack of circumscribed area of hemorrhage
Physical and neurologic exam Skull and spinal radiography CT scan MRI PET
Respiratory support; intubation and mechanical ventilation Seizure precautions and prevention NG tube to manage reduced gastric motility and prevent aspiration Fluid and electrolyte maintenance Pain and anxiety management
Nutrition
Health history with focus on the immediate injury, time, cause, and the direction and force of the blow Baseline assessment LOC—Glasgow Coma Scale Frequent and ongoing neurologic assessment Multisystem assessment
Ineffective airway clearance and impaired gas exchange Ineffective cerebral perfusion Deficient fluid volume Imbalanced nutrition Risk for injury Risk for imbalanced body temperature Risk for impaired skin integrity Disturbed thought patterns Disturbed sleep pattern Interrupted family process Deficient knowledge
Major goals may include: Maintenance of patent airway and adequate CPP Fluid and electrolyte balance Adequate nutritional status Prevention of secondary injury Maintenance of normal temperature Maintenance of skin integrity Improvement of cognitive function Prevention of sleep deprivation Effective family coping Increased knowledge about rehabilitation process Absence of complications
Ongoing assessment and monitoring are vital LOC Vital signs Maintenance of airway Motor function I&O and daily weights Monitor blood and urine electrolytes and osmolality and blood glucose Measures to promote adequate nutrition
Strategies to prevent injury Assessment of oxygenation Assessment of bladder and urinary output Assessment for constriction caused by dressings and casts Pad side rails Mittens to prevent self-injury; avoid restraints Reduce environmental stimuli Adequate lighting to reduce visual hallucinations Measures to minimize disruption of sleep–wake cycles Skin care Measures to prevent infection
Maintaining body temperature Maintain appropriate environmental temperature Use of coverings: sheets, blankets to patient needs Administration of acetaminophen for fever Cooling blankets or cool baths; avoid shivering Support of cognitive function Support of family Provide and reinforce information Measures to promote effective coping Setting of realistic, well-defined short-term goals Referral for counseling Support groups Patient and family teaching
276,000 persons in the United States live with disability from SCI Causes include MVAs, falls, violence (gunshot wounds), and sports-related injuries Males account for 80% of SCIs Average age of injury is 42 Risk factors include; young age, male gender, alcohol and drug use Primary prevention Most frequently involved vertebrae: Cervical – C5, C6, & C7 Thoracic – T12 Lumbar – L1
The result of concussion, contusion, laceration or compression of spinal cord Primary injury is the result of the initial trauma and usually permanent Secondary injury resulting from SCI include edema, hemorrhage, and necrosis Major concern for critical care nurses Treatment is needed to prevent partial injury from developing into more extensive, permanent damage
Tetraplegia (Quadriplegia) Injury occurring between C1 and C8 Paralysis involving all four extremities Paraplegia Injury occurring between T1 and L4 Paralysis involving only the lower extremities
Spinal shock A sudden depression of reflex activity below the level of spinal injury A complete but temporary loss of motor, sensory, reflex, and autonomic function that occurs immediately after injury as the cord’s response to the injury. Muscular flaccidity, lack of sensation and reflexes Usually lasts less than 48 hours but can continue for several weeks
Neurogenic shock Occurs most commonly in clients with injuries above T6 and usually is experienced soon after the injury Caused by the loss of function of the autonomic nervous system Blood pressure, heart rate, and cardiac output decrease Venous pooling occurs because of peripheral vasodilation Paralyzed portions of the body do not perspire
Monitor for signs of shock following a spinal cord injury Monitor for hypotension and bradycardia Monitor for reflex activity Assess bowel sounds Monitor for bowel and urinary retention Provide supportive measures as prescribed, based on the presence of symptoms Monitor for the return of reflexes
stroke! Occurs after spinal shock has resolved and may occur years after the injury Occurs in persons with SC lesions above T6 and in cervical lesions Autonomic nervous system responses are exaggerated Symptoms include severe pounding headache, sudden increase in blood pressure, profuse diaphoresis, nausea, nasal congestion, flushing, and bradycardia Triggering stimuli include distended bladder (most common cause), distention or contraction of visceral organs (e.g., constipation), or stimulation of the skin sre 7
7• Finally, the brain sends messages down the spinal cord to make the blood vessels open up again. S. The rise in blood 6
Unfortunately, the injury
pressure is detected by sensors in the heart and neck called .barorece ptors. These then send signal to the brain. 5 4
6. The brain has two ways it can -- , o p p .o se the rise in blood pressure. fi messages via the parasympathetic vatus nerve to the heart to slo it down.
3. When the impulses to the cord stops these messages, so only the blood vessels above the injury dilate.
tly it sends
This is not enough to overcome the constricted vessels low theinjury level, and so the blood pressure continues to rise.
Nation• • ROfl• bll ;t.aUoi, H06 oit• J THE MYSTERY OF AUTONOMIC DYSREFLEXIA? Autonomic Oys.reflexla (AD)Is amedlcal emergency spe-clflc to lnd lvtd uals wi th Spina! CordInjury(SCI)at the neurological level of T6 or above. It Is usually causedwhen a painfulIrritation occurs below thelevelof yourspinal cordinjvry.It c;anpresent withavariety of signs/ symptoms whichcan vary from mild to severedis.com fort . As a SCIindividual youMed to havea goodunderstanding of AD 11nd be familillr with signsand symptomsl'Jnd immcdit1temanagement of thispotentially life throtuenlngcol\di tion. ll mustbeaddressed immediatel y becauseif it isunheated it mayp,ogress to causea seizure, strokeor death. (Ahr•ms Prestlce 1998).
Bladd &f'
CAUSES HOW DO I GET AUTONOMIC DYSREFLEXIA? SIGNS & SYMPTOMS • Distension (duecocatMUH blocleage or ki nking) • Urina.ry tract Infect ion • 81;:,ddct stone-5 Bowol • ConsU tlon • Ha n hoids • Fissu1e • Havtng boWet car•perfo,med S kin • Pressu,e Uke< • Tigh t Clothing • Ingrown toqn;tll • Blister/burn Others • Scrotalcomprcnion
• • •
S•xu.11 $timulatin Labour Chikl bl t th Men, trvat lon .incl any
@ Atte mp te d compensati on message cannot pass through the spinal cordand blood
AT0'tA90V£ THORACK: LEVEL T 6 @ c ausing high blood pressure
':>\N!:::1\l 1NG cond ition thAt wouJd usually eauseabdominal pain
Emergency Treatment for Autonomic Dysreflexia Signs / SymJ)toms 01 Autooo m k: Oystefk>xla ♦ pressurecontinuesto rise
,::._ @ Irr i tatio n below tho level of SCIsuch as •••·.
.... .. Call rorassistance • Sl t upright a"d lOwe,legs • Loosen any tight c1oth ln9 / legs S-tr...
Similar Free PDFs

Kaplan med surg 2
- 8 Pages

Med SURG; assignment 2
- 9 Pages

Chapter 68-ppt - med surg 2
- 19 Pages

Med surg 2 care plan
- 3 Pages

MED SURG EXAM 3-2
- 54 Pages

Exam 2 Med Surg 2 Practice Questions
- 16 Pages

Common Med Surg Meds
- 7 Pages

Med surg dorris bowman
- 4 Pages

Med surg - notes
- 28 Pages

Med-Surg Endocrine
- 11 Pages
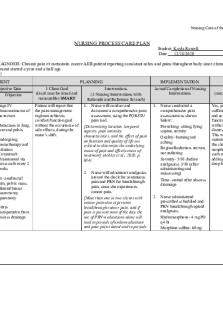
Med Surg- Care Plan
- 6 Pages

Med-Surg Capstone remediation
- 4 Pages

Med Surg Exam 3
- 19 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu


