Kaplan Med Surg 1 2 Comprehensive Rationales.pdf PDF

| Title | Kaplan Med Surg 1 2 Comprehensive Rationales.pdf |
|---|---|
| Author | Jenna Hardin |
| Course | Adult Health Nursing |
| Institution | Jackson State University |
| Pages | 85 |
| File Size | 2 MB |
| File Type | |
| Total Downloads | 2 |
| Total Views | 130 |
Summary
hfjhffdsajkhdfjkhedkgjlkdfjgkh ljkdkagjkfdjakgjafdk jklsdfgklsfdkjfdjgkfdsjgkfdjglk jsdfgkksfdjgklsdfjg jlkgsfdjksfdkgksdfjgkf jigfksdkdfglkjdfskglfkdsjkdfjg gdfjljkfsdlkgjfsdjgfkjsgjk dfgjjdsjfgjfdkgfjskgjkgfjkgdfjlkgfjklgdfjklgjkldfjklgdfsjlkgdfjklgfjksfjklgdfsjklsgdfjk jifdgjlkfdjklfjlkgsdfjdfgsj...
Description
Kaplan→ Med Surg 1, 2 & Comprehensive Rationales Med Surg 1A Topics 1. Cushing’s Syndrome (2 questions) → hypersecretion of ACTH (hormone that allows body to react to stress) ○ https://www.youtube.com/watch?v=ea1sXgd5ui8 ● Signs & Symptoms → fatigue, muscle weakness, weight gain, thinning extremities, thin & fragile skin, moon face & ruddy complexion, hirsutism, truncal obesity, broad purple striae, bruising, impaired wound healing, increased blood pressure & sodium, hypokalemia, hyperglycemia, buffalo hump, DM ● Treatment → restore hormone balance by radiation, drug therapy or adrenalectomy (removal of one or both adrenal glands) ● Nursing Considerations → Frequently monitor VS (especially BP), monitor labs for electrolyte changes, monitor daily weight, check for signs of infection, perform passive range of motion for those that have osteoporosis or are bedridden ○ Post-surgery nursing considerations → encourage coughing & deep breathing, monitor for shock & HTN, administer cortisone as ordered ○ Diet → High in protein & potassium, but low in carbs & sodium, high calcium + vit. D 2. Hepatitis (3 questions) → inflammation of the liver that causes liver cell damage ○ https://www.youtube.com/watch?v=eocRM7MhF68 ○ Chronic hepatitis (> 6 months) can lead to cirrhosis of the liver ● Causes → bacteria, toxins or viruses , 6 viral types → A, B, C, D, E, G ● Hepatitis A & E → fecal to oral (shellfish from contaminated waters is a major source) ● Hep. A stages ○ Pre-icteric: malaise, N/V, anorexia ○ Icteric: jaundice, clay colored stool, tea colored urine ○ Convalescent: SX resolves ● Hepatitis B,C, D & G → parenteral drug abuse, sex, blood & body fluids, ● Signs & Symptoms → jaundice, anorexia, RUQ pain (due to hepatomegaly), clay-colored stools, tea-colored urine (due to bilirubin leakage), apendicitispruritus, elevated LFT’s (AST & ALT) & prolonged PT ● Treatment → symptomatic → vitamin K, anti-histamines, corticosteroids, anti-emetics & apply calamine lotion ● Nursing Interventions → improve sanitation, vaccination, no ETOH, instruct pt to balance rest and activity, patient cannot donate blood! HAND WASHING #1! ● Diet: low in fat, high in carbs and protein 3. Cytoscopy → direct visualization of the urethra, bladder, ureteral orifices, and prostatic urethra ○ https://www.youtube.com/watch?v=eiw8YM4YLFE - for males ○ https://www.youtube.com/watch?v=P0-HXugWdDw - for females ○ Helps assess ureters and the pelvis of each kidney ○ Can obtain a urine specimen from each kidney to evaluate its function ○ Assist in performing a biopsy ○ Assist in removing calculi from the urethra, bladder and ureter ○ Performed in both lower and upper tract ● Lower tract cystoscopy ○ Pt. is usually awake; discomfort is equal to that of catheterization ○ Viscous lidocaine can be injected prior to the study to minimize post-test discomfort
●
●
○ General anesthesia is usually administered Upper Tract cystoscopy ○ Pt. usually kept NPO for several hours before test ○ A sedative may be administered ○ Pt. can expect some burning on voiding, blood in urine, urinary frequency ○ Heat applications are helpful in relieving pain and relaxing muscles Nursing Care → monitor pt. with prostatic hyperplasia (enlarged prostate that can cause urine difficulty) for urine retention, suggest warm sitz baths and antispasmodic meds, monitor for s/s of UTI
4. Diabetes Mellitus (4 questions) → know setting priorities → Condition is characterized by a high level of glucose in the body ○ Signs & Symptoms → THE POLY’s (polyuria,polydipsia, polyphagia), weakness, dizziness, fatigue i. In Children → those above + enuresis (bed-wetting), unusual fatigue & irritability ○ Type 1 → beta cells in pancreas are destroyed and produce no insulin i. Treatment → insulin injections, continuous infusion via pump & diet control ○ Type 2 → beta cells in pancreas secrete insulin, but the body is resistant to its effects i. Treatment → insulin, oral hypoglycemic injections & diet control ○ Diet Management → monitor total calories, carbs & timing of food ○ Diet Intake → meals with complex carbs, ↓ fat, ↑ fiber, some protein i. Time meals with peak effect of insulin ii. Provide extra snacks for unplanned physical activity iii. Substitute soft foods 6-8 times per day if you cannot stick with the usual meal plan iv. If vomiting, diarrhea or fever persist take in some liquids like ½ cup coke, juice, broth or 1 cup of gatorade to maintain caloric intake every ½ hour or hour v. Report nausea, vomiting & diarrhea to HCp → extreme fluid loss = dangerous vi. Unable to retain fluids = hospitalization to prevent DKA ○ Patient Teachings → lose weight if obese, oral hypoglycemic agents, maintain healthy weight, s/s of hypoglycemia & hyperglycemia, self-monitoring of glucose, skin/foot care, importance of exercise ○ “Sick Day” Rules → guidelines for managing diabetes when ill → aimed at preventing DKA i. Take insulin or hypoglycemic agents as usual ii. Test blood glucose & urine ketones every 3-4 hrs → report elevated levels to MD iii. If you take insulin, you may need supplemental doses every 3-4 hours ○ Dawn Phenomena → early morning glucose levels are elevated caused by nocturnal release of growth hormone ○ Somogyi Effect → fall in blood glucose during the night with ↑ morning glucose levels → caused by 5. Thermal Injury (4 questions) ● First degree (Superficial partial-thickness)→ epidermis affected (destroyed or injured); painful, red, dry, min. or no edema ● Second degree (Deep partial-thickness) → epidermis and part of dermis affected; painful, red, exudes fluid, edema, blistered ● Third degree → Total destruction of epidermis, entire dermis, and in some cases subcutaneous tissue, muscle or bone; painless, varied color (white, red, black, brown or charred), dry, leathery,
edema, symptoms of shock, probable hematuria (RBC in urine) and hemolysis (break down of RBC’s) ● First responder interventions: ensure safety of yourself, extinguish flames, cool burn by briefly applying cool water to burn and clothing covering burn, remove other clothing, cover wound to prevent contamination, irrigate chemical burns, asses ABC’s ● Treatment: grafts → use of skin or other materials to cover burned areas ● Nursing Care: IV Lactated Ringers, plasma; F/C to monitor I/O (should be 30ml/hr), check for s/s of fluid overload vs. dehydration, monitor BP, v/s, weight, electrolytes, wound care at least once a day (administer pain meds 30min before wound care), sterile technique, tetanus prophylaxis; high caloric, high-carb, high-protein diet, may require parenteral nutrition; estimate TBSA (total body surface area) with the Rule off 6. Herpes Zoster (Shingles) → Acute infectious viral disease that is reactive of chickenpox virus, presents as unilateral, painful rash, group of vesicles on an erythematous base along a dermatome ○ Treatment → calamine lotion to soothe itching & pain, Acyclovir, corticosteroids to reduce inflammation, vaccination to prevent or modify the disease course ● Nursing considerations: minimize pain & prevent complications, analgesics, apply compresses (wet dressings to skin lesions & cold compresses to ruptured vesicles), administer systemic corticosteroids to diminish severity, prevent spread- contagious to anyone who has not had chickenpox or is immunocompromised 7. Hernia (2 questions → know Umbilical Hernia) → protrusion of intestines through a weakness in the umbilical ring, muscle & fascia Types of Hernias ● https://www.youtube.com/watch?v=3wUrJGDgGO4 ● Umbilical → Hernia occurring at the naval ; more common in women who are obese or multiparous ○ S/S → bulging protrusion at the umbilicus → pain, discomfort at site ○ Treatment → Size of fascial ring less than 2 cm = none; larger = surgery → laparascope ○ Nursing Care → do not use a belly band or tape a silver dollar to the area, keep pressure dressing in place until sutures are healed, sponge-bath child until the dressing is removed & keep diapers folded below the dressing ● Hiatal → opening in diaphragm through which esophagus passes ○ S/S: heartburn, full after meals, GI bleed and N/V (severe) ● Inguinal → Protrusion of the hernia sac containing the intestine of the inguinal opening 8. Incentive Spirometer → Breathing device used to maximize lung expansion by opening closed alveoli and mobilize secretions → facilitates tissue oxygenation!, prevents atelectasis ● Nursing considerations: instruct client to breath in and exhale normally, seal lips around mouthpiece, inhale slowly and deeply, holding breath for at least 3 seconds while keeping ball or cylinder elevate, exhale, take several normal breaths and repeat 4-5 to,es; client should cough after procedure to facilitate secretion removal 9. NG Tube Insertion → Tube from nose into stomach inserted to instill medication ,food, fluids, to remove stomach contents, to obtain specimen for laboratory analysis ● Insertion: ○ Measure distance from tip of nose to earlobe plus the distance from the earlobe to the bottom of the xiphoid process, mark the distance on the tube with tape
○
Lube end of tube with water-soluble lubricant, insert tube through the nose to the stomach; offer sips of water and advance gently; bend head forward to close epiglottis, closing trachea ○ Observe for respiratory distress→ an indication of misplacement in the lungs ○ If in correctly, secure tube w/ hypoallergenic tape and verify placement by evaluating gastric aspirate; aspirate should have pH of =4 ■ If in lungs = resp. distress ○ Different types of tubes: ■ Lebin tube: used for decompression and tube feeding ■ Salem tube: decompression and suction ■ Seng-staken Blakemore tube: bleeding and esophageal varices 10. Diabetic Ketoacidosis → Life-threatening condition in type 1 DM; caused by lack of insulin; body drawing on fat & protein stores for energy; ketone of Na+, Cl-, K+, water, increased RR & urine output, & leads to dehydration & hypoxia ● When acidosis is severe, Pt can lose consciousness (diabetic coma) ○ Indications of impending coma include HA, drowsiness, weakness, confusion, hypotension, tachycardia, warm dry flushed skin, dry mucous membranes, N/V, elevated temperature, polyuria, polydipsia, rapid & deep respirations (Kussmaul’s respirations), fruity odor to breath (from ketone bodies) ● Nursing intervention: administer insulin; IV fluids; electrolytes as ordered; monitor electrolytes status, I&O’s, blood glucose levels; insert & maintain NG tube & urinary catheter as needed ● Teach measures to prevent recurrence such as daily monitoring of blood glucose & monitoring ketones if blood glucose is over 250-300mg/dL, adherence to diabetes management program (including insulin administration), exercise, keeping appointments, recognizing symptoms of infection (a major cause of DKA), & phoning for assistance if symptoms noted 11. Thyroid Disorders (5 questions → know Grave’s disease & Hypothyroid) → ○ Hyperthyroidism → hypersecretion of thyroid gland (Graves Disease) i. S/S → hyperthermia, HTN, tachycardia, heat intolerance, diaphoresis, increased appetite, irritability, muscle fatigue, hyperactivity, sleep deprivation, hyperreflexia ii. Treatment → radioactive ablation, complete or partial removal, anti-thyroid meds 1. Radioactive precautions: flush toilet twice, use gloves, put clothes in radioactive sealed bag, don’t hand wash clothes (machine wash only x 2 on hot) iii. Nursing Care → monitor for thyroid storm, heart failure, cardiac dysrhythmias, quiet environment with little stimulus iv. Patient Education → high protein, carb, vitamin & mineral diet, cool clothes, balance rest & activity, may need hormone replacement therapy ○ Thyroid Storm → hyperpyrexia (fever), cardiac dysrhythmias & altered mental status → hypothermic blanket, O2 & meds to suppress thyroid ○ Hypothyroidism → low secretion or cellular resistance to thyroid hormone i. S/S → weakness, fatigue, unexplained weight gain, constipation, edema, slow pulse rate, decreased libido, infertility ii. Treatment → gradual thyroid replacement with levothyroxine iii. Nursing Care → high-bulk(protein), low-calorie diet & encourage activity ○ Myxedema → patients w/ hypothyroidism i. non-pitting edema in periorbital area & hands/feet caused by severe or long standing hypothyroidism → patient must continue meds for hypothyroidism to prevent this!
12. Immobility Hazards → know hazardous things if patient is immobile ● Includes pressure ulcers, osteoporosis, hypercalcemia, negative nitrogen balance, increased cardiac workload, orthostatic hypotension, stasis of respiratory secretions, boredom, depression ● Nursing considerations: turn frequently, provide good skin care, give high-protein diet with small-frequent feedings, rise from bed slowly, turn, cough,and deep breathe. ROM exercises at least 3x each or as much as pt. can tolerate, high protein diet, vitamin A and C ● Tx: enoxaparin → prevents DVT 13. Diabetes Insipidus → results from a deficiency in circulating ADH (vasopressin) → results from dysfunction of the pituitary gland ○ Signs & Symptoms → extreme polyuria, polydipsia (especially cold, iced drinks), nocturia, ↑ plasma osmolality, urine specific gravity 1.001-1.005, fatigue, dehydration → weight loss, poor skin turgor, dry mucous membranes, constipation, muscle weakness, tachycardia & hypotension ○ Medical Causes → brain tumor, head injury, brain surgery & lithium therapy ○ Treatment → identify cause of diabetes insipidus & treat it! Until cause is identified, give vasopressin or vasopressin stimulate to control fluid balance & prevent dehydration. You may also give thiazide diuretics to ↓ fluid volume by creating mild salt depletion ○ Nursing Considerations → monitor I&O, urine specific gravity, skin condition, check weight daily weight, s/s of hypovolemic shock (BP, HR & respirations) & monitor labs for hypernatremia ○ Complications → hypernatremia, severe dehydration & vasoconstriction 14. Hyperglycemia → elevated blood glucose level, usually associated with diabetes ○ Signs & Symptoms → THE POLY’s (polyuria, polydipsia, polyphagia), vision changes, fatigue/weakness, dry skin, slow healing wounds, recurrent infections, numbness/tingling in hands or feet ○ Treatment → varies depending on which type of diabetes i. Type 1 → insulin injections ii. Type 2 → Diet, exercise, oral hypoglycemic agents ○ Nursing Care → work with patients on management of the disorder & how to prevent acute & long-term complications 15. Hypoglycemia → abnormally low level of glucose in the blood, usually occurs suddenly as a complication of diabetes ○ Signs & Symptoms → sweating, tremors, tachycardia/palpitations, nervousness, hunger, confusion, headache ○ Treatment → give either 15 grams of carbs in the form of candy, juice or sugar, 1 mg subq or IM glucagon, 25-50 mL IV 50% dextrose in water to unconscious patients i. After symptoms resolve, give a snack of protein or starch 16. Liver: Cirrhosis (2 questions) → chronic, progressive liver disease caused usually by alcoholism, but can also be caused by viral infections, toxins, bile stasis or obstruction ○ Signs & Symptoms → indigestion, gas, constipation, N/V, esophageal varices, hematemesis, hemorrhage, ascites, anemia, edema in extremities, JAUNDICE, pruritus, DARK URINE, CLAY-COLORED STOOLS, palma erythemia ○ Treatment → must treat what is causing the cirrhosis! i. Lactalose → for ammonia ii. If ascites → paracentesis iii. Shunts to relieve portal hypertension
○
iv. Liver transplant v. Diet: high carb, high protein Nursing Care → HIGH PROTEIN DIET (high carb in early stages, but in late stages restrict fiber, protein, fat & sodium) & give supplemental vitamins i. Check skin, gums, stool & emesis regularly for bleeding ii. Apply pressure to injection sites iii. Assess fluid retention → daily weight iv. Avoid using soap when bathing patient to prevent skin breakdown v. LABS: low H & H
17. Allergy → hypersensitivity caused by exposure to an allergen, a true allergy will cause production of IgE antibodies ○ Allergic reaction is caused by large amounts of histamine being dispersed throughout the circulatory system → causes vasodilation & edema of the tissues ○ Signs & Symptoms → SOB, wheezing, inflamed airways, itching, congestion, erythema ○ Common allergens → PCN, radiopaque dyes, aspirin, blood components, Toxins (snake, bee, wasp, hornet), food (berries, milk, chocolate, eggs, shellfish, seafood, wheat, nuts) & latex i. High risk populations for latex allergy → spina bifida kids, urogenital abnormalities, spinal cord injuries, multiple surgeries, health-care workers ii. Why spina bifida kids? https://www.ifglobal.org/en/37-temp-news/9-latex-allergies ○ Nursing Care → obtain detailed history, establish airway, administer epinephrine or diphenhydramine in the event of a reaction i. Latex allergy → avoid condoms, balloons, gloves, catheters, brown ace bandages, elastic pressure stockings ii. Do not give d5 LR → causes a reaction ○ Client Education → use of inhaler & epi pen, paint walls, toys should be wood, plastic or metal, remove rugs, move bed away from forced air vent ○ Allergic Rhinitis → allergic rxn that results in watery rhinorrhea, nasal obstruction, sneezing, nasal pruritus i. Nursing Care → Anti-histamines & topical anti-inflammatory drugs ○ Allergen Desensitization → used to treat the allergy when the patient is unable to avoid the allergy. Patient is exposed to larger and larger amounts of allergen in an attempt to change the immune system's response. i. Useful for environmental allergies, mostly ii. Serial injections given → start with small doses and gradually increased iii. Safety → Observe for anaphylaxis, have epi on hand, always keep client in office for 30 minutes ○ Eczema → itchy, red skin rash commonly seen in young children, may ooze and form a crust → can also form as a result of an allergen i. Common causes: milk, wheat, eggs ii. Treatment → avoid allergen, apply astringent solution, corticosteroid cream & antihistamines, keep patient from scratching 18. Dialysis (know AV fistula) → 2 types = Peritoneal & Hemodialysis ○ https://www.youtube.com/watch?v=mi34xCfmLhw → forward to 3:50 ○ Peritoneal → removal of excessive fluids & wastes through the peritoneal cavity by surgically inserted catheter
i.
○
Before procedure → obtain baseline vitals, breath sounds, weight, glucose & electrolyte levels ii. During procedure → infuse 1-2 L of fluid into cavity by gravity using sterile technique, leave fluid in for 20 minutes & then remove it by gravity iii. After procedure → take vital signs, check for respiratory distress, pain or discomfort, assess dressing around catheter for wetness iv. Complications → peritonitis (fever, abd pain & cloudy dialysis drainage, swelling, tenderness, redness or purulent secretions at site), abdominal pain, insufficient return of fluid v. Nursing Care → instruct patient to consume high protein & fiber diet Hemodialysis → removal of excess fluids & wastes by circulating patient’s blood through a semi-permeable membrane that acts as an artificial kidney i. Done through a mature AV shunt, fistula or graft (4-6 weeks old) → created by surgical anastomosis of an artery & a vein (usually radial artery & cephalic vein) 1. Complications→ air embolism, blood leaks, blockage/clotting, contamination & exsanguination ii. Nursing Considerations → check thrill & bruit every 8 hours, do not use that site for BP or blood specimens, assess site for infection, instruct patient to not lift anything heavy on that side or sleep on top of it, monitor closely for hypotension, N/V, malaise, HA, dizziness & muscle cramps
19. Cholecystectomy (2 questions) → surgical removal of the gallbladder to restore biliary flow, can be done either laparoscopic or traditional (T-tube) ○ Before surgery → keep on clear liquids/NPO 24 hours before, assess respiratory status ○ After laparoscopic surgery → monitor wounds & dressings, anesthesia related nausea/vomiting, keep in Semi-Fowlers position, encourage early ambulation, apply heat to right shoulder to alleviate any pain caused by phrenic irritation ○ https://www.you...
Similar Free PDFs

Kaplan med surg 2
- 8 Pages

Med SURG; assignment 2
- 9 Pages

Med surg 1
- 33 Pages

Med surg 2 care plan
- 3 Pages

MED SURG EXAM 3-2
- 54 Pages

ATI Med Surg 1 - ATI
- 22 Pages

Exam 2 Med Surg 2 Practice Questions
- 16 Pages

Common Med Surg Meds
- 7 Pages

Med surg dorris bowman
- 4 Pages

Med surg - notes
- 28 Pages

Med-Surg Endocrine
- 11 Pages
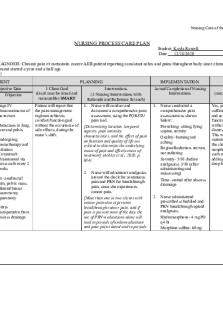
Med Surg- Care Plan
- 6 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu



