Pharmacology Notes for midterm PDF

| Title | Pharmacology Notes for midterm |
|---|---|
| Course | Pharm |
| Institution | The University of Western Ontario |
| Pages | 95 |
| File Size | 5.7 MB |
| File Type | |
| Total Downloads | 41 |
| Total Views | 164 |
Summary
Notes for midterm for the exam that is in November...
Description
1 INTRODUCTION TO PHARMACOKINETICS ● The goal of drug therapy is to prevent, cure or control various diseases ● Elements of the doctor's prescription
●
●
●
●
○ Broad Chemical Classification of Drugs ○ Small Molecules ■ Organic chemicals (natural or synthetic)- note that most of our medications come from nature ■ Molecular weights from 200-900 Da ○ Peptides ■ Up to ten amino acids ■ Small peptidic hormones ○ Proteins –large molecules ■ Enzymes ■ Hormones ■ Antibodies –50 percent of drugs are antibodies ○ Oligonucleotides –get into cells and alters or represses expression of a gene ■ Antisense therapeutics-supress expression of certain types proteins ■ MRNA vaccines Drug Names
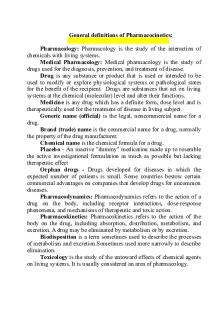
○ Definitions ○ Pharmacokinetics: What the body does to the drug ○ Pharmacodynamics: What the drug does to the body What is Pharmacokinetics ○ Pharmacokinetics (PK) is the quantitative description of drug concentrations in the body over time
2 ■
●
Want to know the concentrations of the drugs in the body and how long it stays in the body ○ The pharmacokinetics of a drug, as it is administered via a specific route in each patient determines, in part the optimum dose (both amount and dosing interval)to be prescribed Relationship between PK and PD
○ ○ ○
●
●
Pharmacokinetics how the dose of the drug effects the blood concentrations Pharmacodynamics is the effects on the body based on the concentration at site of action (concentration at the site of action can be lower or higher than the concentration in the blood) ○ Based on effects and blood analysis you can adjust the dose and intervals of the medications ○ We hardly use the blood concentration to tailor therapy but instead use the concentration at the site of action? Importance of Pharmacokinetics ○ The therapeutic/toxic effects of drugs are related to dose ○ Concentration of drugs in the body at the site of action better relates to drug effects than dose ■ Drug concentration at the site of action is most important...dose and concentration of drug at site can vary among people. Factors that affect this include ● Weight –heavier people tend to have lower distribution ● Sex ● Body composition ○ Therapeutics/toxic effects of drug are related to the concentration achieved in the blood or tissues affected ○ Therapeutic/toxic effects of drugs also relates to the length of time that a chemical persists in blood or tissues Drug Disposition Processes (ADME) and Pharmacokinetic Terms
3
○ ○
○ ○
○
○
○
○
○
Absorption ■ Process by which the drug moves from the site of administration to the bloodstream Distribution ■ Reversible process by which drug moves from circulation to tissues and back Metabolism ■ Chemical conversion of drug administered and it is transform it into another molecule called metabolite usually done by enzymes Elimination ■ Eliminate drug by urine, bile (out liver via bile to gastrointestinal tract), feces ■ Get rid of it from the body Bioavailability ■ The extent of absorption ■ What percent of dose makes it to blood stream Half-life ■ Time it takes for drug to decrease by 50 percent ■ Half-life is related to distribution, metabolism and elimination Volume of Distribution ■ How much of the drug that’s already in body is physically outside of the blood stream ■ Ability to make it to the tissues rather than staying in the blood Clearance ■ A measure of the efficiency of drug removal by the body ■ Drug being metabolised of elimination via urinary or bile
4 ●
○
○
○
What Determines the Pharmacokinetics of a Drug?
■ ■ Concentration depends on ??? Tissue/Membrane Barriers to Drugs-drugs need to pass through barriers ■ Gastrointestinal mucosa ■ Skin, corneal epithelia- can apply drugs into the skin to get it to circulatory system ■ Blood capillaries ■ Placenta ■ Cells of the organs
■ ■ All ADME processes are dependent on drug movements across membranes Pathways for Membrane Permeation
■ Passive Membrane Diffusion ■ Drug is transferred down a concentration gradient, i.e.. from high to low concentrations ■ The membrane plays a passive role; no energy is required beyond that necessary to maintain its integrity
5 ■
○
○
○
Rate of drug transport is proportional to the concentration gradient and frequently follows first-order (linear) kinetics; Rate of transport = k x Conc ; where K is a first-order constant ■ Processes is independent of the presence of other compounds ■ Transport is determined by the physicochemical properties of the drug, particularly lipophilicity and degree of drug ionization Passive Membrane Diffusion and Fick's Law
■ Physicochemical Properties of Drugs that Favour Diffusion Across Biological Membranes ■ Small size (molecular weight10g) will cause saturation of sulfation and glucuronidation pathways, leading to enhanced oxidative bioactivation by CYP enzymes to a toxic metabolite (N-acetyl-p-benzoquinoneimine, NAPQI). NAPQI is efficiently eliminated by GSH conjugation, but when liver GSH is depleted (overdose), hepatotoxicity occurs. N-acetylcysteine is the antidote which is thought to replete liver GSH stores
DRUG TRANSPORTERS ● Membrane Transporters Influence Drug Absorption and Elimination
○ ■
○
○
Epithelial cells have transporters that absorb or eliminate (uptake or efflux transporter) ■ Where on the cell the transporter is located ● One side of the cell faces the blood stream (basal lateral side of the cell) and the other side faced some cavity (apical membrane or brush boarder membrane) In the intestines, uptake transporters on the apical (luminal) side of enterocytes promote drug absorption into the body while efflux transporters on the apical membrane impede drug entry into systemic circulation In the liver, high activity of uptake transporters on the basolateral (blood) side and efflux transporters on the apical (bile) side of hepatocytes promotes excretion into bile and thus prevents high systemic levels of drugs
35 ○
●
In the kidney, high activity of uptake transporters on the basolateral (blood) side and efflux transporters on the apical (urine) side of tubular cells promote excretion into urine and thus prevents high systemic levels of drugs Membrane Transporters Affect Distribution of Drugs into Tissues
● ■
●
High activity of uptake transporters on the blood side of capillary endothelial cells promotes tissue entry of xenobiotics ■ High activity of efflux transporters on the blood side of capillary endothelial cells prevent xenobiotic entry into tissue ■ In the blood brain barrier ● Blood side is called luminal and abluminal faces neurons and whatnot ● There are many efflux transporters on the luminal side of the epithelial cell which makes drug entry to the brain difficult Major Drug Transporter Families ○ Uptake Transporters ■ Solute Carrier, SLC Transporters ■ These transporters function in either a facilitated uptake mechanism or an antiport mechanism
■
●
● ● ○
Organic Anion Transporting Polypeptides (OATP) ○ They transport anions and neutral drugs and even cations (less selective) Organic Anion Transporters (OAT) Organic Cation Transporters (OCT)
Efflux Transporters ■ All of them require ATP and energy (active transporters)
36
■
■ ■ ■
●
(ATP-binding Cassette, ABC Transporters) Highly expressed in cancer cells resisting drugs Also present in non-cancerous cells to move around endogenous solutes ● P-glycoprotein (P-gp, MDR1) ● Multidrug resistance proteins (MRP) ● Breast Cancer Resistance Protein (BCRP) Drug Uptake Transporters
●
○ Drug Efflux Transporters
37
●
○ Renal Drug Transport Mechanisms
○ ○
●
A variety of uptake and efflux transporters are expressed in proximal tubular epithelia ○ Inhibition of renal secretory transporters is cause for several drug-drug interactions ■ Penicillin urinary excretion is inhibited by probenecid (blocks OATs) ● Allows penicillin to stay in the body longer and take drug less frequently ■ Digoxin urinary excretion is inhibited by quinidine (blocks P-gp; MDR1) Pharmacokinetics affects each part of a doctor's prescription
38
○ PHARMACODYNAMICS 1 ● What is Pharmacodynamics? ○ Pharmacodynamics is the quantitative description of the effect of a drug on the body ○ Most (but not all) drugs exert their exert by binding to specialized macromolecules (I.e. receptors, enzymes) ●
The Relationship Between PK and PD
○ ●
Receptors- The Basics
○ ○
Drugs can be thought of as signals that we send to the cell
39 ○ ○
Receptors can be thought of as the detectors, that detect the signal In the simplest schematic, when receptors reside empty, they do not influence intracellular processes ○ When a drug is bound to a receptor, the receptor becomes activated and produces a biological response ○ Many drugs mimic endogenous ligands, some drugs block receptors *** Note- a ligands is a molecule that binds to a receptor. A ligands can be a drug or an endogenous molecule ● Types of Interactions Between Drugs and Receptors
○ ○ ○ ○ ●
Rarely is it one type of bond that causes drug receptor binding, rather it is usually a combination of bonds Generally many weak bonds make up a drug-receptors interaction ■ Van der Waals and hydrogen bonds most common Ionic and covalent interactions are rare
Example: Imatinib Binding to Bcr-Abl Kinase
○ ○ ○
Drug molecule needs to have a certain shape and conformation to fit into the receptor Lot lots amino acids that contribute to the binding
40 ○
●
Most bonds are hydrogen and van der Waals forces
The Relationship Between Drug Concentration and Receptor Occupancy
○ ○
Most drug binding events obey the law of mass action such that...
1.
○
○
●
There are several assumptions that we make when we use this model. They include: 1. All receptors are equally accessible to drugs 2. Binding is reversible 3. Neither the drug or the receptor is altered by binding ● However drug binding to receptor causes a conformational change
The law of mass action: the rate of a chemical reaction depends on the concentration of the reactants
The Equilibrium Dissociation Constant (Kd)
41
○ ○ ○
Kd is the equilibrium dissociation constant and represents the affinity of a drug-receptor pair Kd is calculated as Koff/Kon
■
○ ●
Kd is most often influences by its off rate (Koff) more than its on rate (Kon)
The Equilibrium Dissociation Constant (Kd)
○ ○
○ ○
●
The Kd is expressed in units of concentration (I.e. nM or uM) and is the concentration of drug that occupies half the receptors that occupies half the receptors at equilibrium A small Kd (kd is in units of concentration) means the receptor has a high affinity for the drug and a large Kd means the receptor has a low affinity for a drug The Kd represents the concentration at which 50% of the available receptors are occupied by the drug
Fractional Receptor Occupancy
42 ○ ○
It is often useful to know what fraction of receptor is occupied by a drug In order to look at this we must assume that the total number of receptors is constant. This is usually the case but there are some circumstances where the total number of receptors changes (I.e. certain disease states and repeated exposure of certain drugs)
○ ●
Drug-Receptor Binding is Saturable ○ Cells have a finite number of receptors ○ AQs we increase the dose, more drug-receptor complexes are formed ○ Eventually, increasing the dose does NOT lead to an increase in drug-receptor complexes ○ Dose response curves form a rectangular hyperbola. There are difficult to analyze mathematically ○ Log transforming the X-axis changes the hyperbolic curve into a sigmoidal curve. There are easier to analyze mathematically and are used in pharmacology
○ *** Note- Bmax is the maximum number of binding events *** Note- The red and blue lines represent two different drugs that bind to the same receptor ●
Dose Response Curves ○ There are two main types of dose response curves, quantal and graded 1. Graded- shows the continuous relationship between dose and response ● Ie blood pressure example
43 2. Quantal- Shows the effect of various doses of a drug on the response of a population. Used to describe "all or none" relationships (ie. Death)
●
Graded Dose-Response Curves
○ ■
■
The above figure shows graded dose response curves for 2 different drugs. Notice the similarity between the dose-response curve and the drug-receptor binding curves we looked at earlier! In many (but not all) situations, the magnitude of response is directly related to the amount of drug that occupies its receptor. Similarly, in most cases (but not all), the Emax occurs when all receptors are bound to drug. In these cases the EC50 = Kd. The exception: spare receptors (more later).
○ ●
Potency
○ ○ ○
The amount of drug required to produce an effect of a given magnitude The EC50 is used to determine a drugs potency. The lower a drugs EC50, the more potent it is
44 ○
●
Efficacy
○ ○ ○ ●
●
Example; Ibuprofen vs Acetaminophen ■ Ibuprofen is more potent but both drugs are equally effective at relieving headache ■ Because advil has 200mg per tablets and tylenol has 325mg per tab
The ability of a drug to elicit a response when it binds to its receptor A drugs efficacy is dependent on the number of drug-receptor complexes
Therapeutic Importance: Potency vs Efficacy ○ Your patient is in extreme pain. Which analgesic would you suggest? ○ Drugs with a higher efficacy are generally thought to be more therapeutically beneficial than drugs with a high potency
○ Spare Receptors
45
○ ○ ○
○ ○ ○
●
Up until now we have assumed that 100% receptor occupancy is required to exert maximal effect. In some instances this is not the case! Sometimes less than 100% occupancy results in maximal effect. This discrepancy is described by the presence of “spare receptors”. Notice how in this situation the EC50 is less than the Kd. Spare receptors can be thought of as receptors in excess of those required to produce a full effect. There is nothing different about spare receptors! They are not hidden or different from other receptors.
Spare Receptors Continued
○ ○ ○ ○
How can maximal efficacy be achieved with sub-maximal drug- receptor binding? Amplification of intracellular signals! In the example below, binding of the first three drugs (left side) results in amplification of a signal inside the cell (blue dots inside the cell). Notice how the binding of the 4th and 5th drugs (right side) do not cause amplification of the signal.
46 ○
●
Quantal Dose-Response Curves
○ ○ ○ ○ ●
This demonstrates how the some drugs may reach maximal effect before all the receptors are bound to drug.
Plots of fraction of the population that responds to a given dose of drug NOT graded, the patient either responds or there don't (ie. All or none) Let's do an experiment to see how quantal dose response curves work
Quantal Dose Response Curves
○ ■
○ ○
●
Therapeutic effect and toxic effect are different processes so those that have a high dose for therapeautic effect don’t necessarily need a high concentration for toxic effect You can examine therapeutic effects, toxic effects and lethal effects using quantal dose-response curved The doses that produce the response in 50% of the population are known as the ED50 (effective dose), TD50 (toxic dose) and LD50 (lethal dose)
Therapeutic Index ○ The therapeutic index is an indicator of a drugs relative safety
47 ○
It is calculated as the ratio of the doses of drug that cause toxicity (or lethality) to the doses that produce therapeutic effects ■
○ ●
The larger the therapeutic index, the safer the drug
Therapeutic Index
○ ■
When is it acceptable to use a drug with a small TI? ● Must look at risk/benefit ratio
PHARMACODYNAMICS 2 ● Types of Drug Receptor Interactions:
●
● Agonists ● ● ●
An agonist binds to a receptor and produces a measurable biological effect. An agonist may mimic the response of an endogenous ligand. When an agonist binds to a receptor it stabilizes the receptor in a particular conformation (usually the active conformation)
48
● ○ ●
Means activated???
Full Agonists
● ● ● ● Partial Agonists:
Drugs that bind to their receptor and are able to produce the maximal biological response are considered full agonists. Full agonists have high intrinsic activity (i.e. they are able to maximally activate the receptor). Full agonists stabilize receptors in their fully active conformation
49
○ ○ ○ ○ ○
●
Are molecules that bind to the receptor but only produce a partial response, even when all the receptors are bound. Partial agonists have an intrinsic activity less than that of full agonists. Partial agonists can also act as antagonists since they may block the binding of full agonist ligands. Example: Tamoxifen is a drug used to treat breast cancer. It is a partial agonist of the estrogen receptor
Antagonists: ● "One who opposes or contents another"
● ○ ○ ○
Antagonists inhibit the action of agonists Antagonists have an affinity for receptor but has no intristic effect Antagonists have no effect in the absence of an agonist.
50
●
○ Antagonists that bind to receptors have affinity but no intrinsic activity ● Competitive Antagonist:
○ ○ ○ ○ ○ ○ ○ ○ ○ ●
Bind to the same site on the receptor as the agonist. Has affinity but no intrinsic activity. Binding is reversible, so adding more agonist will overcome the effect of a competitive antagonist. Notice that the presence of an antagonist causes a parallel rightward shift in the dose response curve Competitive antagonists increase the EC50 but do not affect the maximal efficacy. Many drugs act clinically as competitive antagonists. Examples include acetaminophen, statins, and beta receptor blockers Can always get back to maximium ethicacy with an increase in dose of agonost Antagost alone will not produce a response
Measuring Competitive Antagonism:
51
○ ○ ○ ○ ○
To determine competitive binding, you can perform an experiment where you use a single concentration of agonist and vary the concentration of competitive antagonist. This allows you to determine the IC50, the concentration of antagonist required to produce 50% inhibition (i.e. the functional strength of the inhibitor). The IC50 can be misleading because it is dependent on the experimental conditions. ○ Type of anatgonist you are using (each one binds differntly) We can ...
Similar Free PDFs

Pharmacology Notes for midterm
- 95 Pages

Pharmacology Midterm
- 19 Pages

Notes for midterm 1
- 5 Pages

Notes for midterm
- 7 Pages

Notes for Midterm 1
- 33 Pages

Pharmacology notes
- 9 Pages

Notes for midterm - Graeme Metcalf
- 12 Pages

Midterm Notes for Art History
- 27 Pages
Main terms for pharmacology
- 9 Pages

UWorld for Nclex Pharmacology
- 16 Pages

Pharmacology Notes 3
- 2 Pages

Clinical Pharmacology Notes
- 3 Pages

Pharmacology Notes (BREX Lecture)
- 71 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu


