Week 8 - Lecture notes 8 PDF

| Title | Week 8 - Lecture notes 8 |
|---|---|
| Course | Nursing Care 3 - Med & Surgical |
| Institution | The University of Notre Dame (Australia) |
| Pages | 6 |
| File Size | 167.2 KB |
| File Type | |
| Total Downloads | 113 |
| Total Views | 218 |
Summary
- lecture notes from powerpoint expanded on with tutorial notes and information from lecture recording...
Description
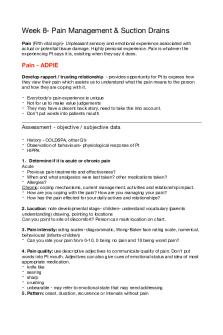
Week 8- Pain Management & Suction Drains ! Pain (Fifth vital sign)- Unpleasant sensory and emotional experience associated with actual or potential tissue damage. Highly personal experience. Pain is whatever the experiencing Pt says it is, exisiting when they say it does. !
Pain - ADPIE Develop rapport / trusting relationship - provides opportunity for Pt to express how they view their pain which assists us to understand what the pain means to the person and how they are coping with it. !
-
Everybody's pain experience is unique Not for us to make value judgements They may have a decent back story, need to take this into account. Don’t put words into patients mouth!
Assessment - objective / subjective data !
- History - COLDSPA, other Q’s! - Observation of behaviours- physiological response of Pt ! - HIPPA! 1. Determine if it is acute or chronic pain Acute! - Previous pain treatments and effectiveness? ! - When and what analgesics were last taken? other medications taken?! - Allergies?! Chronic: coping mechanisms, current management, activities and relationship impact. ! - How are you coping with the pain? How are you managing your pain?! - How has the pain effected for your daily actives and relationships? ! 2. Location: note developmental stage- children- understand vocabulary (parents understanding) drawing, pointing to locations! Can you point to site of discomfort? Person can mark location on chart. ! 3. Pain intensity: rating scales- diagrammatic, Wong-Baker face rating scale, numerical, behavioural (infants-children)! - Can you rate your pain from 0-10, 0 being no pain and 10 being worst pain? ! 4. Pain quality: use descriptive adjectives to communicate quality of pain. Don't put words into Pt mouth. Adjectives can also give cues of emotional status and idea of most appropriate medication. ! - knife like! - searing! - sharp! - crushing! - unbearable - may refer to emotional state that may need addressing ! 5. Pattern: onset, duration, recurrence or intervals without pain!
Identify when pain began, how long it lasted, if it reoccurs, when it last occurred and how long intervals without pain are. ! 6. Precipitating factors: certain actives precede pain, help prevent pain and determine its cause. ! Eg. Physical exertion may precede chest pain, eating > abdominal pain, emotional stresses > migraines, rheumatoid conditions > cold weather.! 7. Alleviating factors: what makes the pain better or worse. ! E.g Home remedies, rest, herbal teas, hot/cold packs, distraction methods (TV/music)! 8. Associated symptoms: address symptoms ! E.g nausea, vomiting, dizziness, diarrhoea! 9. Effect on ADL’s: persons perspective on how pain impacts aspects of their normal functioning. ! E.g. Sleep, concentration, appetite, marital relationships, driving, mood ! 10. Coping resources: Strategies the Pt can use, encourage Pt to use methods. ! E.g religious or cultural influences, solitude, prayer, support networks ! 11. Affective responses: refers to Pt’s interpretation of pain. Nurses explore these responses to treat their mental issues. ! E.g anxiety, fear, exhaustions, depression (chronic pain)! 12. Observation of behavioural and physiological responses: ! - Facial expressions - clenched teeth, tight shut eyes, biting of lower lip, grimacing, crying, screaming ! - Immobilisation of body- holding limb, position, reflexive/jerking ! - Behaviour- confusion, restlessness, aggressive, foetal position !
Diagnosing !
- Acute or Chronic pain ! - Location of pain! - Other associated factors: hopelessness, anxiety, ineffective coping, ineffective health maintenance, insomnia! E.g ineffective airway clearance related to weak cough secondary to postoperative incisional abdominal pain! E.g Impaired physical mobility related to arthritic pain inane and ankle joints. !
Planning and Interventions !
Planning - Established goals should be personalised! - Acknowledge and accept clients pain- listen to Pt, pain is unique, prompt action on needs when addressing pain- options, plan for relief! - Team approach involving the Pt and support persons ! Pharmacological - Opioids, narcotics, NSAIDS, co-analgesic drugs, PCA! Non-pharmacological interventions - body: massage, heat/cold, diet/nutrition, electrical stimulation (TENS)! - mind: relaxation, hypnosis, distraction, info about pain- reduce stress ! - Spirit: prayer, meditation, rituals! - Social interactions: communication, family therapy, volunteering, support groups! - Distraction methods ! Educate Pt Reducing fear and anxiety- relieve strong emotions capable of amplifying pain, give Pt opportunity to talk about their perception and reaction to the pain. Often related to uncertainty about future. Provide accredited info, clarify expectations to minimise anger, answer any Q’s and concerns. ! Preventing pain- managing pain in terms of preventions ! - Pre-emptive analgesia-prior to procedures in order to treat pain before it occurs.! E.g. prior to dressing changes, mobilising, repositioning#post op, removing drains! Ensure you are passing on the information so that pts aren’t having to repeat their story multiple times
Evaluate care! Using goals identified in planning stage, collect data and evaluate effectiveness of interventions and whether or not they satisfy the goals. ! Did it resolve their pain, did the pain score drop, is the Pt more comfortable ! - Diary or flow sheet used for chronic pain- eg. Weekly log with activities, pain onset, times of day, treatments! - Determine effectiveness of pain management ! - Modify/update care plan accordingly ! - Handover!
- Is Pt receiving adequate support?! - Has Pt physical condition changed?! - Is adequate analgesia being given? Would Pt benefit from change in dose?!
Suction Drains Closed Drain System !
Closed drain system reduces possible entry of microorganisms (inserted during surgery) into the wound. ! - Drainage tubes sutured in place and connected to bottle that usually has low suction (suction stopped from 3-5 days postop)! - Allows for accurate measurement of drainage to monitor what and how much is draining.! - Monitoring the suction aids in removing excess exudate that may interfere with granulation of tissue- wound needs to heal from bottom up (not just the surface)! - When emptying bottle, use PPE (gloves, goggles), measure amount of drainage accurately into another container, clean port with alcohol swab, re-establish suction according to type of drain! - Most bottles are disposable – change the whole bottle rather than empty bottle & reuse! - Removed under order from Dr or Surgeon !
Indications for closed wound drainage tube - Abscessed cavity - prevent premature closure, promoting healing from the bottom up and preventing surface layer from healing over. ! - Insecure intra-abdominal wound- compromised healing, DXT (Deep xray radiotherapy), malnourished! - Anticipated exudate- tissues that contain minute secretory glands- liver, pancreas! - Risk of peritonitis- bowel, gastric, biliary surgery, facilitates drainage of content ! - Extensive dissection- large collections of fluid/blood ! - Traumatic injury- to drain contaminants! Types of drains - Jackson-Pratt™ – soft pliable tube with multiple perforations with a bulb that can recreate low negative pressure vacuum, designed so body tissues are not sucked into the tube, decreasing risk of bowel perforation. Often used in abdo.! - Redivac™ / Varivac ™ / Haemovac ™- high negative pressure drain. Dial up the suction according to doctors orders (3 stages). The bunny ears tell you if there is suction (crossed= pressure). Used commonly for knee surgery.! - Pigtail™– Small lumen with a coil, used for draining a single cavity. Passive drain, easily blocked. Maintain patency by flushing 1-2 times daily. Self retaining (no suture). Must be ‘uncoiled’ prior to removal by cutting releasing string first, otherwise, severe pain and tissue damage may occur. ! - Penrose™– flat ribbon-like drain, gauze is applied to external end to absorb drainage, can be colonised by bacteria if left in situ for an extended period of time.! Nursing considerations / principles of management - Client/carer support & education- eg. mobility and care! - Prevent infection!
- Ensure drain is Secure! - Maintain patency of drain - shouldn’t be any kinks, occlusions, clamps! - Maintain skin integrity - dressing changes as per hospital quality, keep surrounding skin clean!
- Contain exudate ! - Observe type & amount of exudate! - Observe for complications: discomfort, infection, dislodgement, blockage, if negative -
pressure- loss of suction, loss of skin integrity ! Refer to the hospital policy/unit guidelines for removal (watch video on blackboard)!
Suction Drain removal ! Ensure plan in place - Documented by medical team that it is safe to remove- check order ! - Note type of drain removal requirements eg. pigtail etc! - Explain procedure and gain consent! - Give pre-analgesia prior to removal (approx. 45mins prior)! - Some drains recommend turning off suction 3-5mins prior to removal (Varivac). ! Procedure- aseptic technique - Clean site first and remove anchoring suture/s with a stitch cutter! - Gently move drain to loosen; remove the drain in a smooth, continuous motion! - Tie off purse string sutures if present! - Send tip of drain for cultures to pathology if required! - Apply an occlusive, & absorbent dressing! - Monitor site for bleeding and swelling ! Document- removal and drainage amount on FBC and in progress notes !
Negative pressure wound therapy / vacuum assisted wound healing (VAC)! The use of controlled negative pressure wound therapy to assist and accelerate wound healing.#! - Speeds tissue healing by reducing swelling around the wound! - Enhancing wound healing by providing a moist, protective environment! Sterile foam sponges are placed into clean wound and covered with a transparent adhesive drape (opsite), a hole is cut to allow insertion of vacuum tubing. Suction can be continues or intermittent. !
Negative Pressure Wound Therapy Systems - Controlled topical negative pressure is applied to the entire wound. - Foam dressing is changed every second day. - Continuous therapy for the first 48 hrs. - Followed by intermittent therapy (5min on / 2min off) for increased granulation tissue formation.
Benefits of negative pressure wound drains - Increased local, functional blood perfusion to the area - Increased nutrient delivery to wounded tissue - Accelerated granulation - Decreased wound bacterial counts - Reduces localised oedema - Moist environment aids in contraction and facilitates epithelialisation! EXTRAS PICC / CVC - Complication during insertion of the CVC- puncture parietal layer causing pneumothorax ! - PICC line or CVC if they are not flushed- can become blocked with residue. Can result in infection and blood clots. ! - Education regarding care of their PICC line prior to discharge! • Always clean your hands before and after you come in contact with any part of the PICC! • Keep the PICC dry! • Watch for signs of infection- redness, pain, inflammation, heat, fever ! EXTRAS- PCA - Safety features- Drug library, Different delivery modes, Cassette for additional security, Ambulatory design, Delivers via SC route usually, Ambulatory design, Locked plastic box/container! ADPIE for IDC care A •Bladder scans pre/prior to installation of fluid! •Monitor and assess drainage! •BP, Temp, Pulse ! • Perineal area care- monitor, educate Pt prior to insertion ! D: Day 1 post TURP (Transurethral removal of prostate) ! P: Goals Maintaining normal urinary elimination! • Promoting fluid intake! • Preventing Urinary Tract Infections (UTI) ! Managing urinary incontinence! • Bladder training - clamp catheter to see if Pt can pass urine voluntarily ! • Pelvic floor exercises - reduces episodes of incontinence ! • Maintain skin integrity - prevent moist skin and pressure ulcers ! I •Empty bag every shift! •Take shower instead of baths! •Monitor signs and symptoms of UTI! •FBC ! E: Assessment of current patient status at expected outcomes - is urine clear? Pain, urine output – did you nursing care work for your patient to achieve nursing / medical goals...
Similar Free PDFs
Week 8 - Lecture notes 8
- 6 Pages

Week 8 - Lecture notes 8
- 23 Pages

WEEK 8 - Lecture notes 8
- 10 Pages

Week 8 - Lecture notes
- 3 Pages

GBCM Week 8 - Lecture notes 8
- 8 Pages

Week 8, Part 2 - Lecture notes 8
- 5 Pages

8 - Lecture notes 8
- 21 Pages

8 - Lecture notes 8
- 21 Pages

4 - Lecture notes Week 8
- 2 Pages

8 Midwifery - Lecture notes 8
- 3 Pages

Taxation 8 - Lecture notes 8
- 2 Pages

Week 8 Lecture
- 51 Pages

Dox 8 - Lecture notes 8
- 21 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu


