Med Sur Care plan SBAR George PDF

| Title | Med Sur Care plan SBAR George |
|---|---|
| Course | medical surgical |
| Institution | Jersey College Nursing School |
| Pages | 18 |
| File Size | 422.4 KB |
| File Type | |
| Total Downloads | 105 |
| Total Views | 190 |
Summary
care plan ...
Description
Data Collection and Care Plan Patient (Code) Full Age 54 Primary MD: Howard MRN: 1868054 Room: 401 Steele, M.D. Harry George Sex: Male Primary Diagnosis: Cellulitis left foot with osteomyelitis, type 2 diabetes mellitus, alcoholism Past Medical History Past Surgical History 1. Fracture left foot 4 years ago. 2. Chronic infection to left foot. 3. Type 2 Diabetes Mellitus. 4. Alcohol abuse. 5. 2-pack-per-day smoker for 36 years.
Repair of fractured metatarsals and left malleolus 4 years ago.
CODE Status: Full Vital Signs: Time Monday: 0705
T (tympanic )101.4 F
AP
110 R 24
B/P 146/88 R 24
O2 Sat 94
Pain: (0-10) Allergies: Wt.145ls Unknown medication for urinary tract infection-- Ht. 5ft 11in causes rash. GI/Nutrition Normal: • Bowel sounds active in all quadrants Abdomen
5
Admission date: Monday
Abdominal examination: a. Inspection: Mildly swollen abdomen, no pulsations observed b. Auscultation: Bowel sounds in four quadrants c. Palpation: No tenderness, no masses Diet: 1. Usual appetite: "Not bad" 2.Current appetite: Poor. "Haven't felt like eating for last week." 3. Do you have any dietary restrictions or problems we should know about: No 4. Have you had any recent weight gains or losses: No 5. Oral cavity: a. Teeth/dentures: Full teeth, some chipped b. Dental caries: Many c. Gums: Dark pink, swollen. Patient reports they bleed easily. d. Oral mucosa: Pink, dry e. Lesions: None f. Altered taste: No
6. Eating patterns: a. Food preferences, allergies, intolerances: None b. Number of meals/day: One c. Special diets: No d. Dietary supplements: No e. Difficulty swallowing or chewing: No f. Fluid intake: Mostly vodka g. Can you eat independently: Yes h. Do you need help preparing meals: No i. Can you afford food and utilities for cooking: No j. Appetite changes (describe): No k. Nausea and vomiting (describe precipitating/relieving factors): No 7. Any history of GI, liver, or endocrine problems: No How did you assist the client with their diet? No assistance
•
•
soft, non-distended, non-tender Receives and tolerates nutrition and fluids Absence of nausea, vomiting, cramping, diarrhea or Constipation No complaints of nausea, vomiting, or abdomen pain with palpation
Describe your Findings: Negative history for GI symptoms. No food allergies. Has been eating one meal a day at homeless shelter for the last few months, when he can. Reports normal bowel function.
Intake: Patient consumed 50% of meal Neurological • Normal Findings: • Alert and oriented x 3 • Speech is clear • Memory intact • Follows commands and converses • Absence of seizures • Behavior appropriate to situation • When upright: Balance steady Gross motor coordination intact • Hand grasps strong/equal • PERRLA, • Foot presses and pulls strong and equal • Gag, cough, blink reflexes intact • Patient denies numbness tingling or other paresthesia of extremities
Describe your findings: NEUROLOGIC: Alert and oriented x 3. Cranial nerves intact. Glascow Coma Scale--15. No difficulty with speech. Appropriate response to questions. Responds appropriately to commands. Denies problems with headaches, dizziness, tremors, or numbness Memory: a. Short-term: Poor, concentration impaired b. Long-term: Able to recall relevant events from past 7. Decision making: Has been poor. States has made some poor decisions, and that is why he is in the state he is in today. 8. Speech and voice patterns:Normal 9. Alternate form of communication: None 10. Neurologic changes: None 11. Vision (describe impairments): None 12. Visual aids: None 13. Hearing: Normal 14. Auditory aids: None 15. Taste, touch, smell: Normal HEENT:
Respiratory • Normal Findings: • Breath sounds clear and equal in all lobes. • Respirations regular, non-labored, without use of accessory muscles • Mucous membranes pink • Chest excursion symmetri cal Trachea midline • If cough present, nonpersistent • Sputum clear or absent Cardiovascular • Normal Findings: • Regular rhythm, heart sounds S1 S2 present • Blood pressure WNL • Denies chest pain • Periorbital, sacral, pedal & generalized edema absent • Skin warm & dry to slightly moist • Nail beds pink, capillary refill< 3 sec • Pulses palpable or present with doppler Skin • Normal Findings: • Color within patient's norm • Temperature warm, dry to slightly moist • Turgor normal, mucous membranes moist • Intact without breakdown, rash,
Holds head normally. Skull symmetrical, smooth. No deformities. Moves freely without discomfort or dizziness. Hair--dirty with flakiness all over. Skin-leathery with numerous healed scars on left face from nose to ear. Face--symmetrical. External auditory meatus--normal size. Large amount cerumen in ear canals. Tympanum normal. Hearing normal. No nasal deviation. Oral cavity pink, dry. No difficulty swallowing. Teeth--fair condition. Thyroid normal. Trachea midline. No lymphadenopathy. Describe your findings: LUNGS: Chest contour symmetrical. A/P diameter normal. No bulging or movement noted in intercostal spaces. Clear to auscultation with normal breath sounds. Admits to "smoker's cough" for years. Pulmonary: No history of pneumonia, tuberculosis, or COPD. Has never been tested for tuberculosis. No apparent respiratory difficulty. Has been a 2-PPD smoker since age 18.
Describe your findings: HEART: Auscultation of heart--no murmurs or clicks. Normal S1 and S2. No extra sounds. Normal sinus rhythm with tachycardia. JVD negative. Cardiac: No history of heart disease. Is not complaining of any chest pain. Has never been told he had heart disease or hypertension.
Describe your findings: Skin assessment: a. Integrity: Dry and leathery, especially on face. 2 cm open wound on left foot with redness, swelling, and serous drainage. b. Turgor: Poor c. Rash, incisions (describe location, size, healing): Incision left foot and open lesion with drainage d. Varicosities: No e. Poor wound healing: Yes, left ankle
redness, blanching Wounds: • Normal Findings: • Edges approximated and clean • Surrounding tissues free from signs & symptoms of infection • Dressing dry & intact: drainage absent
f. Drainage: Serous drainage left ankle g. Bruising: No h. Lesions: Left malleolus i. Petechiae: No j. Lymph node assessment as indicated: Palpable inguinal lymph nodes bilaterally k. Condition of hair and nails: Unkempt hair with flakiness and brittle ragged nails SKIN: Face leathery with healed scars. Skin dry and intact except on left foot as described above. BACK: Normal spinal curvature. No scars or lesions.
Wounds: (yes/no?) Findings: Yes as noted above Mobility/Functional Ability Musculoskeletal: Denies problems with bones or joints except for pain in • Normal Findings: left foot EXTREMITIES: • Active ROM of all extremities within Thin legs. Pulses present on right. Unable to palpate pulses in left dorsal physical limitations pedis or posterior tibial, because of swelling. Adequate popliteal and • Tolerates prescribed activity femoral on left. Left foot edematous, reddened with serous exudate. Did order not test gait. ROM normal in cervical spine, shoulders and upper arms. • If ambulatory, gait steady Describe your findings: • Able to complete ADL's Limitations in activities of daily living: • Able to transfer Difficulty walking since foot became sore (with/without assistance) 10. Ability to perform activities of daily living (ADL): • Assistive device(s) correctly ADL Neurovascular assessment for Eating: independent client with cast or traction Dressing: independent Ambulating: independent Toileting: independent Bathing: independent Grooming: independent Writing: independent Cooking: independent Cleaning: independent Shopping: independent Doing laundry: independent Taking medication: independent Managing money: independent 11. Limitations in mobility: Limp because of sore left foot 12. List assistive devices: None 13. Muscular weakness or fatigue: Left foot 14. Swelling, redness, or warmth around joints or over muscles: Swelling, redness left foot, toes to midcalf 15. Gait: Limp
16. Range of motion in limbs: Normal in right upper and lower and right lower extremity, but limited in left lower extremity 17. Sensation: Decreased sensation both lower extremities. Difficulty distinguishing sharp versus dull.
GU/Elimination
Describe your findings:
•
1. Last bowel movement: Day before yesterday 2. Stool characteristics: "Normal" 3. What is your pattern of bowel movements: Daily 4. Laxatives or bowel elimination aids: No 5. Any surgeries pertinent to bowel elimination: No 6. Abdominal examination: a. Inspection: Mildly swollen abdomen, no pulsations observed b. Auscultation: Bowel sounds in four quadrants c. Palpation: No tenderness, no masses 7. How often do you urinate: 6-8 times a day 8. Any problems with continence: No 9. Urine color/character of urine: Yellow GU: Reports normal voiding patterns. No noticed blood in urine. 10. Any catheter (check one): Indwelling 11. Bladder distention: No 12. Usual urinary pattern: a. Nocturia: No b. Dysuria: No c. Hematuria: No d. Poor or interrupted stream: No e. Straining: No f. Stress incontinence: No g. Hesitancy: No h. Frequency: Sometimes i. Urgency: No j. Pain (identify area, such as groin, abdomen, flank/kidney, perineal): No 13. Alterations from normal urinary patterns: None 14. Use of protective devices: No 15. Previous treatment for urinary tract infections: Years ago, treated with pill that caused rash
Normal Findings: • Urine clear, straw or amber no unusual color • Urine output within established parameters • Bladder non distended • Patient is incontinent of urine of uses a collection device.
Output:60 ml/hr
Psycho-Social •
Normal Findings: • Participates in two-way conversation, care and treatment plan • Able to communicate his/her needs • Coping mechanisms intact (client and family) • Mood/affect/behavior appropriate to situation
Describe your findings: 1. Patient's description of self: "A loser." States "need to get my act together" s 2. Effects of illness or surgery on self-concept: Great effect for last 4 years. Led to drinking pr 3. Recent stressful life events or life-changing eve 4. Verbalizes feelings of fear or anxiety: Fear about never seeing boys again 5. Source of anxiety or fear: Pain and life situation
6. Physical manifestations of stress/anxiety: Nervousness, heavy smoking and drinking 7. Perception of abilities: Poor. Used to be good construction worker. 8. Body posture: Lying in bed 9. Eye contact: Good 10.Barriers to learning: None 11. Best method for instruction: Demonstration 12. Primary language: English a. Read (check one): Yes b. Write (check one): Yes c. Understand (check one):Yes 13. Memory: a. Short-term: Poor, concentration impaired b. Long-term: Able to recall relevant events from 14. Decision making: Has been poor. States has made some poor decisi the state he is in today. 15. Speech and voice patterns: Normal 16. Alternate form of communication: None 17. Neurologic changes: None 18. Vision (describe impairments): None 19. Visual aids: None 20. Hearing: Normal 21. Auditory aids: None
Comfort, Rest and Sleep • • •
•
Rates pain as 0 States and appears rested Rests/sleeps during shift Slept well during night
Describe your findings: 1. Do you have any problems sleeping or resting? Yes. Patient states he doesn't always have a bed t bridge or on park bench. 2. Patterns of sleep: Irregular. Has never been able to get more than 3. Sleep routines: When he can get it. Much better when in shelter. 4. Patient's perception of quality of sleep: Not too bad when has a place to sleep 5. Patterns of rest and relaxation: Not much 6. Patient's perception of their energy: Better before foot became sore 7. Sleep aids (pillows, medication): None 8. Exercise and recreational activities: None Pain Assessment: 1. Are you currently experiencing pain, or do you Severe pain in left foot 2. Pain/discomfort: a. Pain onset: Is continuous without medication b. Rating (scale of 0 to 10; 0 = no pain): 10 c. Duration: Most of time d. Location(s): Left ankle e. Quality: Intense aching and sometimes throbb
Safety: Describe your findings:
Diagnostic Testing/Laboratory Data: Laboratory Results DAY/TIME: Mon 1500 HEMATOLOGY WBC 19,200 RBC 5.0 HEMOGLOBIN 14.2 HEMATOCRIT 44 MCV 98 PLATELETS 350,000 DIFF: NEUTROPHIL SEGS 65 NEUTROPHIL BANDS 15 LYMPHOCYTES 16 MONOCYTES 4 EOSINOPHILS 0 BASOPHILS 0 RETICULOCYTES 0.2 ERYTHROCYTE SEDIMENTATION RATE 36 NEUTROPHILS 80 CHEMISTRY GLUCOSE 380 SODIUM 145 POTASSIUM 5.1 CHLORIDE 107 CO2 18
f. Radiation: Foot to toes g. Aggravating or associated factors: Constant an walk h. Alleviating factors: Vodka 3. Nausea: None 4. Social isolation: Yes, except for "guys" at hom If Restraints used: Describe care 1. Infection risk: High risk 2. Fall risk: High risk 3. Physical injury, bodily harm, or hurt: a. Injuries: High risk for injury because of foot b. Trauma: Low c. Skin integrity: High risk because of potential i d. Tissue integrity: High risk e. Dentition: Potential high risk because of poor f. Suffocation: No risk g. Aspiration: No risk h. Airway clearance: No risk i. Neurovascular function: Moderate risk becaus Mellitus j. Evaluate cranial nerves: No risk 4. Violence: None 5. Environmental hazards: Living situation 6. Temperature regulation: Fever with infection 7. Impact of disabilities on safety: High risk beca
CREATININE 1.0 BUN 18 URIC ACID 4.8 CALCIUM 10 PHOSPHORUS 1.8 ALBUMIN 2.8 ALKALINE PHOSPHATASE ALT (SGPT) 86 AST 80 (ENDOCRINE HBA1C 9.0 URINE COLOR Dark amber CLARITY Turbid GLUCOSE 4+ KETONES Moderate SP GR 1.030 BLOOD Neg pH 6.8 PROTEIN 6 mg NITRITE Neg LEUKOCYTES (ESTIMATED) Few MICRO: WBC Few RBC Neg BACTERIA Neg DAY/TIME: Mon 1500 COAGULATIONS PT 11.5 INR 1.2 PTT 38 FIBRINOGEN FSPSGOT) 80
Teaching Needs Identified during the assessment: 1. Pain assessment. 2. Pain management. 3. Effects of alcohol on body. 4. Withdrawal effects (from alcohol). 5. Effect of smoking on healing. 6. Treatment and care of type 2 diabetes. 7. Medications-Glyburide and antibiotics. 8. Asking for assistance before attempting to get out of bed. 9. Getting up and ambulating safely. 10. Use of bathroom handrails and call light. 11. Safe use of a wheelchair.
Teaching reinforced: 1.Asking for assistance before attempting to get out of bed.
2. Getting up and ambulating safely. 3. Use of bathroom handrails and call light. 4.Safe use of a wheelchair. Goal # ITEM TAUGHT
1 2 5 8 9-11
Pain scale Hydromorphone hydrochloride Smoking-healing How to call nurse for help Performing ADLs safely with physical limitations
PERSON TAUGHT
INITIAL TEACHING
TEACHING REINFORCEMENT DATE LE Tue Tue
P P
DATE Mon Tue
LEVEL 1 1
P P
Tue Mon
1 1
Tue Tue
P
Tue
1
Tue
Key Codes for Patient/Family Teaching: Teaching Assessment/Final Evaluation Level: 1 = has no knowledge/skill 2 = has some knowledge/skill 3 = demonstrates knowledge/skill with supervision 4 = demonstrates knowledge/skill consistently and independently N/A = no longer applicable
Person(s) Taught: P = patient PT = parent GP = gr S = spouse OF = other family O = others (please specify):
SBAR report: Situation: My name is Natalee Burrell, LPN Patient: Harry George Room: 401 MRN: 1868054
Physician: Howard Steele, M.D.
Admission date: Monday Reason for this admission as stated by patient/chief complaint: "My foot has been killing me and nothing helps the pain." Background: Admitting Diagnosis: Cellulitis left foot with osteomyelitis, type 2 diabetes mellitus, alcoholism. dressing in place over ankle, small amount Peripheral IV infusing Normal saline at 125 ml/hr. Foley catheter in place to gravity drainage, adequate amounts of vital signs: T 100.6, BP 138/88, P 99, RR 20. Blood glucose continues to be elevated. Sitter in attendance at bedside. Assessment:
Harry agitated and tremulous intermittently throughout the night. Resting at intervals after Chlordiazepoxide given restlessness, and occasional combativeness upon awakening from sleep. Complaining of severe pain 10/10 in left foot 0715. Left foot red and swollen with decreased sensation and movement. Left foot elevated on 2 pillows. Thin legs. P Unable to palpate pulses in left dorsal pedis or posterior tibial, because of swelling. Adequate popliteal and femoral o reddened with serous exudate. Did not test gait. ROM normal in cervical spine, shoulders and upper arms. Recommendation: Stronger medication for worsening pain. Hydromorphone. Wound culture to identify causative organism of wound i Team to assess and treat patient wound. Physical therapy and evaluation for impaired gait and mobility. Check folic lipase, repeat CBC and electrolytes. Schedule bone scan for today.
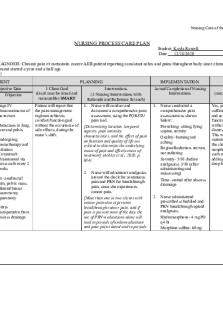
Professional Nursing Care Plan The following table provides information to utilize in developing your nursing care plans. Each column in the care plan from should include the appropriate information related to the Nursing Diagnosis. You are expected to develop 3 Nursing Diagnoses with the supporting documentation as noted on the page below. The Nursing Diagnoses are then labeled in priority order where 1 would be the highest priority. (Nursing Diagnosis Priority # ) Any questions that you have concerning the nursing care plans should be directed to your instructor.
(I) Data Collection Related to the Nursing Diagnosis Subjective (Nonobservable)
(II) Complete NANDA Nursing Diagnosis
(IV) Nursing Interventions
Objective (Observable)
Subjective data should be clear, concise and specific to the Nursing Diagnosis
Objective data should be clear, concise and specific to the Nursing Diagnosis
Subjective Data:
Objective Data :
What the patient or
What is observed or
family relates,
measured. May
states, or reports. (Non-
include the client’s behavior, vital
• •
•
•
Choose a NANDA approved diagnosis. The statement should list only one diagnosis and listed in the following format, i.e., problem followed by "Related to (R/T) the disease process Manifested by: (signs and symptoms) is not part of nursing diagnoses and should be written as a separate line. Example: Coping, ineffective family: R/T Temporary family disorganization and role changes. Manifested by significant other's limited personal communication with client. Each statement should be supported by a rationale
(III) Goals/Outcomes (Long and Short term) Including timelines/timeframes
Should be: • Concise • Clear • Specific • Individualized • Accomplishable client and/or family, significa other.
• observable)
signs, lung sounds, urine output, laboratory data, diagnostic testing
Could have both short term and long term outcomes throughout NCP, but each client should have one long term goal as part of the NCP. Definitions: Short-term goals: Those goals that are usually met before
(etc.) as related to the specific nursing
discharge or before transfer to a less acute level of care. Long-term goals: Those goals that may not be achieved before
diagnosis.
discharge but require continued attention as by client and/or
(Observable)
significant others as indicated. •
Each diagnosis, if appropriate, could have short-term goals and
•
long-term goals. Statements: Specific - relates to nursing diagnosis. Measurable - tells what to see, hear, or smell.
Achievable - realistic for patient....
Similar Free PDFs

Med Sur Care plan SBAR George
- 18 Pages
Med Surg- Care Plan
- 6 Pages

Med surg 2 care plan
- 3 Pages

Mental Health SBAR Plan of Care
- 4 Pages

UTI Care Plan - Care Plan
- 7 Pages

Care plan 3 - Care Plan
- 3 Pages

Care Plan 1 - Care plan
- 7 Pages

Care Plan 2 - Care plan
- 21 Pages

SBAR - SBAR
- 1 Pages

N101L Care Plan - Nursing Care Plan
- 11 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu





