Mental Health Care Plan PDF

| Title | Mental Health Care Plan |
|---|---|
| Course | Mental Health Competencies |
| Institution | Texas Woman's University |
| Pages | 8 |
| File Size | 336.3 KB |
| File Type | |
| Total Downloads | 65 |
| Total Views | 146 |
Summary
Mental Health Care Plan example...
Description
N 4615 Clinical Worksheet 2018 1
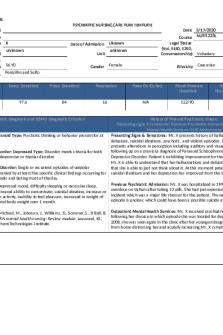
Care Plan/Clinical Worksheet N4615 Age 71 Gender Male Legal status: Involuntarily
Highest Grade Completed:
High School
Instructions: Initial information for pages 1 & 2 should be taken from the chart. This information can then used to complete the rest of the worksheet/care plan. Client's Complaint (use verbatim from the chart): Sunday, a neighbor across the street told me.”
Past admissions (dates):
“My father was murdered on
He was hospitalized at Ben Taub 5 years ago.
History of Present Admission (Date, events leading up to admission, and mode of admission: Patient was bought by police for erratic behavior, found at a neighbor's property shaking the fence.
Client’s stated understanding of diagnosis: “I was out of whack.”
Laboratory (Identify important areas. Medications that have hepatic, renal, cardiovascular, endocrine, or other system implications address those labs): Date/Test
Result
Interpretation
Nursing implication
2/20/2020
6.8 ug/ml-
Normal level
Check blood levels during treatment or when changing
Carbamazapine 2/20/2020
normal 4.79
Normal level
dose; therapeutic level 4-12 mcg/ml. Monitor for thyroid level since carbamazepine might
TSH
mU/L-
2/20/2020
normal Negative
RPR
decrease thyroid hormone level. Normal level
Monitor lab for sexually transmitted disease associated with increase in sex drive during manic episodes.
DSM-V Diagnosis: Admitting Diagnosis: features. 01/16 v1
Bipolar disorder I, most recent episode manic, with psychotic
N 4615 Clinical Worksheet 2018 2
Methamphetamine use disorder. Medical Illnesses: Irritable bowel syndrome, left arm infection. Psychosocial issues: drug use Physical assessment: (Not a formal head-to-toe assessment.) [e.g., Any problems breathing? Coughing? When was your last bowel movement? Any burning sensations when you empty your bladder?] Record data from chart indicating a problem, indicate any current changes data. From chart: Height:
5 feet 10 inches
Weight:
200
BMI: (calculate if not available) Vital signs:
29
BP: 122/76 Pulse: 113 RR: 18 Temp: 98.3 SpO2: 98%
Skin, Hair Nails:
No clubbing. He does have a tattoo to his extremity, his face. He does
have wounds noted to bilateral ACs, but they are dry. There is no oozing. No apparent rash, lesions, abrasion, or laceration. Head and neck: Normocephalic, nontraumatic. No thyromegaly. Trachea is midline. Endocrine:
Normal TSH level
Cardiovascular:Regular rate and rhythm. S1, S2 clear. No murmurs. Muscular-Skeletal:
Negative decondition, back pain or joint pain.
Respiratory:
No coughing. No shortness of breath. No wheezing.
Gastrointestinal:
He says he was having diarrhea, but he has IBS. He says,” My
doctor told me to take imodium.” He said he feels better. Negative for abdominal pain. No constipation. Genitourinary: Negative burning urination, dysuria, or frequency. No genital lesions.
01/16 v1
N 4615 Clinical Worksheet 2018 3
Psychiatric Medications: Generic Name
1. Quetiapine (Seroquel) 2. Carbamazepine (Carbatrol) 3. Venlafaxine (Effexor)
Dosage Include prescribed dose with time and maximum dose 50mg H.S. at 2100 300mg TID 75mg A.S.
4. required. See the last 3 pages of this care plan.
01/16 v1
Route
Specific use for this Client and
Side-Effects Food/Drug Interactions
therapeutic levels when applicable
Include CNS, Integumentary, Musculoskeletal, GI, GU, Endocrine, CV, Renal, Hepatic, Psychiatric
Oral
To help patient sleep
Avoid alcohol, effects of alcohol and medication can intensify
Oral
For Bipolar disorder
Oral
Nursing Implications include for each side-effect and drug interaction
Monitor for unusual behavior changes
N 4615 Clinical Worksheet 2018 4
Clinical presentation (textbook description) of Admitting Diagnosis. “Bipolar I disorder is the diagnosis given to an individual who is experiencing a manic episode or has a history of one or more manic episodes. The client may also have experienced episodes of depression. This diagnosis is further specified by the current or most recent behavioral episode experienced. For example, the specifier might be single manic episode (to describe individuals having a first episode of mania) or current (or most recent) episode manic, hypomanic, mixed, or depressed (to describe individuals who have had recurrent mood episodes). Psychotic or catatonic features may also be noted (Townsend and Morgan, 2018, pg. 535).” Mental Status on day of care: Provide evidence (examples) for each category and indicate any change from admission MSE. USE DIRECT STATEMENTS FROM THE PATIENT, not summary statements. Appearance: Patient appears to be well-groomed, multiple tattoos covers both arms and neck. Mood & Affect (give data and note if congruent): “I’m fine.” Patient mood and affect seem to be congruent. The patient seems calm and is laughing with the nursing staff. Memory Recent & Remote (evaluate and provide verifiable examples): “Today is February 29, 2020.” “It is a leap year.” Thought Process &Content (provide examples of each to support findings): When asked what his psychiatric diagnosis of schizophrenia means to him, the patient stated, “I was out of_wack,____ police brought me in.” Insight & Judgment (provide examples of each to support findings): When discussing why the patient was brought into the hospital and his use of drugs, the patient stated, “I’m not doing meth anymore.” Developmental Level: Identify developmental levels for the theorist listed. Additionally, students are to choose a 3rd theorist that most appropriately defines the client’s needs and one that would be used by the nurse to provide care. Please provide complete information for the three theorists. Theorist Maslow:
Level Safety and security
Erikson:
Ego integrity vs despair
01/16 v1
Supporting Data The patient was at risk for injury from having altered cognitive and sensory perception. “Safety needs. Once physiological needs are met, the safety needs take precedence. The safety needs include security; protection; freedom from fear, anxiety, and chaos; and the need for law, order, and limits (Varcarolis, 2017, pg. 23).” The patient had a delusion that his father was
N 4615 Clinical Worksheet 2018 5
murdered by the CIA when in reality, his father passed away a long time ago. He was ambivalent about his sexual identity. He reported having a husband. Then a minute later, he reported wanting to have kids with his wife. His ego and grieving capability were impaired. “Danger—lack of generativity results in selfabsorption and stagnation (Varcarolis, 2017, pg. 22).” Other: Beck
Cognitive distortion: Negative expectations of the environment
Patient has a delusion that his father was murdered by the CIA. “These cognitive distortions arise out of a defect in cognitive development, and the individual feels inadequate, worthless, and rejected by others. Outlook for the future is one of pessimism and hopelessness1. (Townsend and Morgan, 2018, pg. 504).”
. How does the client's culture impact his or her mental health needs at this time? (it always does) Patient did not identify any way in which culture impacts his mental health. ______________________________________________________________________________ How does the client’s spirituality impact his or her mental health needs at this time? (may be formal religion, or simply sense of meaning and hope) Patient is atheist.
Patient will be coming to classes at Bellaire Behavioral Hospital every day for his PHP program for substance use. He expressed__________ understanding about his discharge plan and seems willing to participate.
How is the client participating in Treatment Plan?
Nursing Process: Refer to your text for essential elements of documentation. Include mood, affect, and behavior as well as physiologic data in the assessment. Problem List: (Please list all current mental and medical issues for this client. Prioritize the list before completing the plan of care. Use appropriate nursing diagnosis when building the problem list. When prioritizing use Maslow and think about how the problems may inter-relate. In providing care and working on the priority diagnosis first other issue may be alleviated.
Client Problem
Priority
1. Disturbed thought process
1
Assessment data Patient has flight of ideas, responds to internal stimulation, tangential speaking patterns and has
2. Substance Use
2
delusion. Patient injected methamphetamine IV for the past 5 or 6 years. He had wounds from injection on left and right arm
01/16 v1
N 4615 Clinical Worksheet 2018 6
Rows should be added for clients with more than 8 identified problems. The list should include medical needs as well. Remember when the physiologic become a higher priority than the psychological issue the patient will be transferred to a medical hospital (this is not the patient to use for your care plan. Priority Nursing Diagnoses: 1. Nursing Diagnosis (Problem R/T Etiology or Human Response R/T Stressor) Disturbed thought process related to psychosis and substance abuse. Data supporting Problem: (AEB) Patient has flight of ideas, responds to internal stimulation, tangential speaking patterns and has delusion. Expected Outcomes (include short term objectives that demonstrate measurable progress to major goal(s): Short term: Patient appropriately interacts and cooperates with staff and peers in therapeutic community setting before discharge. Long term: Patient uses coping strategies to deal effectively with hallucinations/delusions during follow-up. Nursing Interventions (make specific to individual and useful to nurses that come after to you to care for patient; w/ Rationale): https://nurseslabs.com/substance-abuse-nursing-diagnosis-careplan/ 1. Provide safety measures (e.g., side rails, padding, as necessary; close supervision, seizure precautions), as indicated. Rationale: It is always necessary to consider the safety of the patient. 2. Maintain a pleasant and quiet environment and approach the patient in a slow and calm manner. Rationale: Patient may respond with anxious or aggressive behaviors if startled or overstimulated. 3. Present reality concisely and briefly and do not challenge illogical thinking. Avoid vague or evasive remarks. Rationale: Delusional patients are extremely sensitive about others and can recognize insincerity. Evasive comments or hesitation reinforces mistrust or delusions. 4. Encourage the patient to participate in resocialization activities/groups when available. Rationale: This is to maximize level of function.
01/16 v1
N 4615 Clinical Worksheet 2018 7
5. Refer to community resources (e.g., day-care programs, support groups, drug/alcohol rehabilitation, mental health treatment programs). Rationale: These measures are necessary to promote wellness. Nursing Process continued: Plan: a) Immediate plan: Patient is being discharged today (2/29/20), so the plan is to receive two
weeks of medications, understand discharge plans, and go home with partner. ________________ _____________________________________________________________________________________ b) Discharge planning and use of community resources: _Patient will attend a follow up appointment at Bellaire PHP and also attend the PHP program__
for substance use every day. Patient is going home with partner.__________________________ ____________________________________________________________________________________ Actual Outcome: (How is client different from morning report): Patient was reported to be doing well since the night shift. There has been no change in patient. He is calm.
01/16 v1
N 4615 Clinical Worksheet 2018 8
C.R.
01/16 v1...
Similar Free PDFs

Mental Health Care Plan
- 8 Pages

Mental Health Clinical Care Plan
- 1 Pages

Mental Health SBAR Plan of Care
- 4 Pages

UTI Care Plan - Care Plan
- 7 Pages

Care plan 3 - Care Plan
- 3 Pages

Care Plan 1 - Care plan
- 7 Pages

Care Plan 2 - Care plan
- 21 Pages

Mental Health
- 44 Pages

N101L Care Plan - Nursing Care Plan
- 11 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu