X answers Nursing Care Plan mental health PDF

| Title | X answers Nursing Care Plan mental health |
|---|---|
| Author | Jan Flores |
| Course | clinical |
| Institution | West Coast University |
| Pages | 21 |
| File Size | 859.3 KB |
| File Type | |
| Total Downloads | 62 |
| Total Views | 155 |
Summary
Mental Health Nursing Care Plan for patient X with answers to help guide your journey through clinical rotations online....
Description
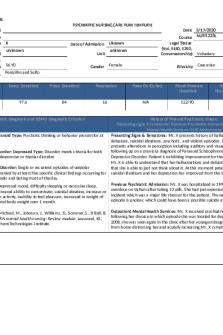
Course: NURS 223L PSYCHIATRIC NURSING CARE PLAN TEMPLATE
Student Instructor Patient Initials X Patient DOB Chronological and Apparent Age Allergies
Date of Admission
unknown
Unit
56 YO
Gender
Date 5/17/2020 Course NURS 223L Legal Status (Vol, 5150, 5250, Conservatorship) Voluntary
Uknown unknown Female
Ethnicity
Caucasian
Penicillin and Sulfo
Height/Weight
Temp (location)
Pulse (location)
Respiration
209.8 lbs.
97.6
84
16
Psychiatric Diagnosis and DSM 5 Diagnostic Criterion
Schizophrenia: Paranoid Type: Psychotic thinking or behavior present for at least 6 months. Schizoaffective Disorder: Depressed Type: Disorder meets criteria for both schizophrenia and depressive or bipolar disorder. Major Depressive Disorder: Single or recurrent episodes of unipolar depression accompanied by at least five specific clinical findings occurring for a minimum of 2 weeks and lasting most of the day. Clinical Findings: Depressed mood, difficulty sleeping or excessive sleep, indecisiveness, decreased ability to concentrate, suicidal ideation, increase or decreased in motor activity, inability to feel pleasure, increased in weight of more than 5% of total body weight over 1 month.
Pulse Ox (O2 Sat)
N/A
Blood Pressure (location) 122/90
Pain Scale 1-10 (location, character, onset) N/A
History of Present Psychiatric Illness: Presenting signs & symptoms/ Previous Psychiatric Admission / Outpatient Mental Health Services/5150 Advisement Presenting Signs & Symptoms: Ms. X presents history of hallucinations, delusions, suicidal ideations, psychotic, and violent episodes. In addition, patient presents alterations in perception including auditory and visual. Ms. X is following up on a previous diagnosis of Paranoid Schizophrenia and Major Depressive Disorder. Patient is exhibiting improvement for the past few months. Ms. X is able to understand that her hallucinations and delusions are unreal and that she is able to just not think about it. At this moment patient doesn’t exhibit suicidal ideations and her depression has improved from the last visit Previous Psychiatric Admission: Ms. X was hospitalized in 1993 following an overdose on Valium after taking 13 pills. She had just experienced a robbery incident which was a major life stressor for the patient. The nature of the episode is unclear, which could have been a possible suicide attempt.
Holman, H. C., McMichael, M., Johnson, J., Williams, D., Sommer, S., & Ball, B. Outpatient Mental Health Services: Ms. X received psychiatric help in 1991 following her divorce in which episode she was treated for depression. In August S. (2019). RN mental health nursing: Review module. Leawood, KS, 2008, she was seen again in the clinic after her youngest daughter moved out FL: Assessment Technologies Institute. from home distressing her and acutely increasing Ms. X symptoms.
Page 1 of 21
Course: NURS 223L PSYCHIATRIC NURSING CARE PLAN TEMPLATE Erickson’s Developmental Stage Psychopathology of admitting and/or related psychiatric diagnosis Include Rationale Based on the Patient Biophysical and/or related medical diagnosis Description of how this diagnosis relates to your patient With APA citations With APA citations Paranoid Schizophrenia, Paranoid Type: Ms. X has a history of delusions and Generativity vs. Stagnation: Erickson’s developmental stage which occurs hallucinations for more than 6 months. To support the paranoid type the approximately between 45-65 years old, at this time adults strive to nurture patient has history of some degree of paranoid delusions with frequent things by parenting children and contributing to society by doing things to auditory hallucinations in initial presentation which includes her affect as not benefit future generations which is important for the generativity versus prominently flat. This findings supports the paranoid type of schizophrenia. stagnation stage of development. Generativity referring to caring for others while creating and accomplishing things that will make the world a better place. On the other hand, stagnation is the failure to find a way to contribute. As seen Schizoaffective Disorder: This diagnosis best explains Ms. X’s symptomatology which meets criteria for schizophrenia and depressive on Ms. X case these individuals are usually disconnected with society as a whole. disorder. Patient states that she lives in an apartment by herself and that her social life is very limited. In addition, Ms. X sees herself as someone who does not like people invading her space. The information acquired from Ms. X refers that she Major Depressive Disorder: Ms. X seems to have met at least 5 of the 9 symptoms at some point in her life. belongs to the stagnation stage of Erickson’s Developmental Stages.
Ms. X has a family history of paranoid behavior by her father, and depression by her mother appeared to be a possible genetic link for the disorders. Holman, H. C., McMichael, M., Johnson, J., Williams, D., Sommer, S., & Ball, B. S. (2019). RN mental health nursing: Review module. Leawood, KS, FL: Assessment Technologies Institute.
Page 2 of 21
Cherry, K. (2019, July 17). The Differences and Characteristics of Generativity and Stagnation. Retrieved from https://www.verywellmind.com/generativity-versus-stagnation-2795734
Course: NURS 223L PSYCHIATRIC NURSING CARE PLAN TEMPLATE
Presenting Appearance (nutritional status, physical deformities, hearing impaired, glasses, injuries, cane) Basic Grooming and Hygiene (clean, disheveled and whether it is appropriate attire for the weather) Presenting Appearance: Appeared stated aged, good eye contact. Basic Grooming and Hygiene: Well groomed
Interpersonal Characteristics and Approach to Evaluation (oppositional/resistant, submissive, defensive, open and friendly, candid and cooperative, showed subdued mistrust and hostility, excessive shyness)
Attitude: Calm, cooperative Patient states that she understands her past paranoia and hallucinations are unreal. Abstraction: Good
Page 3 of 21
MENTAL STATUS EXAMINATION Appearance Gait and Motor Coordination (awkward, staggering, shuffling, rigid, trembling with intentional movement or at rest), posture (slouched, erect), any noticeable mannerisms or gestures Gait and Motor Coordination: Not noticeable
Manner and Approach Behavioral Approach (distant, indifferent, unconcerned, evasive, negative, irritable, depressive, anxious, sullen, angry, assaultive, exhibitionistic, seductive, frightened, alert, agitated, lethargic, needed minor/considerable reinforcement and soothing). Coping and stress tolerance.
Behavioral Approach: Calm, concerned Coping and stress tolerance: Ms. X has history of not coping well with major life stressors. One major distress for Ms. X occurred in August 2007 when her youngest daughter got married and moved out on her own causing the patient to exhibit psychotic symptoms.
Level of Participation in the Program/Activity (Group attendance and milieu participation, exercise)
Level of Participation in the Program/ Activity: Ms. X states she exercises during her lunch breaks and follows a healthy diet, which have been helping her in improving her mood, sleep, and occupational functioning. Patient will be refer to interpersonal and family therapy. Speech (normal rate and volume, pressured, slow, loud, quiet, impoverished) Expressive Language (no problems expressing self, circumstantial and tangential responses, difficulties finding words, echolalia, mumbling) Receptive Language (normal, able to comprehend questions, difficulty understanding questions) Speech: Clear, normal rate, rhythm, and volume Ms. X speaks fluently and prefers English as her language of choice. Patient is able to carry a conversation without bringing up psychotic delusions or hallucinations. Receptive Language: Patient did not bring up topics or any psychotic symptoms until specifically asked. Ms. X seems to understand that occasionally hearing sounds from the woods or hearing someone crying outside her apartment are not real, and she lets them go after only mentioning one.
Course: NURS 223L PSYCHIATRIC NURSING CARE PLAN TEMPLATE
Recall and Memory (recalls recent and past events in their personal history). Recalls three words (e.g., Cadillac, zebra, and purple) Orientation (person, place, time, presidents, your name) Recall and Memory: Within normal limits, MMSE: 30/30 Orientation: Patient oriented x 3. Oriented to person, place and time.
Orientation, Alertness, and Thought Process Alertness (sleepy, alert, dull and uninterested, highly distractible) Coherence (responses were coherent and easy to understand, simplistic and concrete, lacking in necessary detail, overly detailed and difficult to follow) Alertness: Ms. X is alert and oriented. Coherence: Noted delusional thinking, relating to everyday noises to other issues as per HPI.
Concentration and Attention (naming the days of the week or months of the year in reverse order, spelling the word "world", their own last name, or the ABC's backwards)
Concentration and Attention: Within normal limits Patient states: “Focus at work is much improved”. Cognitive: Not formally tested but grossly within normal limits. Serial Seven shown no errors
Thought Processes (loose associations, confabulations, flight of ideas, ideas of reference, illogical thinking, grandiosity, magical thinking, obsessions, perseveration, delusions, reports of experiences of depersonalization). Values and belief system
Hallucinations and Delusions (presence, absence, denied visual but admitted olfactory and auditory, denied but showed signs of them during testing, denied except for times associated with the use of substances, denied while taking medications)
Judgment and Insight (based on explanations of what they did, what happened, and if they expected the outcome, good, poor, fair, strong)
Thought Processes: Logical and goal directed
Hallucinations and Delusions: Patient main delusion in the past was believing that she birthed children that she never known. Ms. X persistent delusions include thinking that someone around her apartment looks like her daughter, but will not allow her to get closed to her to see who she is. Patient relates this delusion to her thinking that she had unknown children, but she is able to rationalized that this may not be real and states that she is able to not think about it all the time.
Judgment: Good Ms. X see herself as a normal person, who does not trust others. Patient is aware that her delusions and hallucinations may not be real. Insight: Fair
Values and Belief System: Ms. X states that she has spiritual beliefs possibly associated with seeking forgiveness from God. However, she currently attends church now and then and is not making it a cornerstone of her life now.
Mood or how they feel most days (happy, sad, despondent, melancholic, euphoric, elevated, depressed, irritable, anxious, angry). Affect or how they felt at a given moment (comments can include range of emotions such Page 4 of 21
Mood and Affect: Rapport (easy to establish, initially difficult but easier over time, difficult to establish, tenuous, easily upset) Facial and Emotional Expressions (relaxed, tense, smiled, laughed, became insulting,
Response to Failure on Test Items (unaware, frustrated, anxious, obsessed, unaffected) Impulsivity (poor, effected by substance use) Anxiety
Course: NURS 223L
as broad, restricted, blunted, flat, inappropriate, labile, consistent with the content of the conversation. Mood: Mildly depressed. Ms. X depression has improved from her last visit were she was a 3/10. Patient states that her mood is stable as long as she remains busy. Affect: Congruent with mood
Risk Assessment: Suicidal and Homicidal Ideation (ideation but no plan or intent, clear/unclear plan but no intent) Self-Injurious Behavior (cutting, burning) Hypersexual, Elopement, Non-adherence to treatment Suicidal/ Homicidal Ideation: No suicidal or homicidal ideation present. Patient states that her mood is stable and denies any suicidal or homicidal ideation. Past history of possible suicide attempt does not seem to cause a probable recurrence.
Page 5 of 21
PSYCHIATRIC NURSING CARE PLAN TEMPLATE yelled, happy, sad, alert, day-dreamy, angry, smiling, distrustful/suspicious, tearful, pessimistic, optimistic)
Rapport: Candid and easy to establish It is expected for the clinician to establish and maintain rapport with this patient. Facial and Emotional Expressions: Presentation includes her affect as not prominently flat.
(note level of anxiety, any behaviors that indicated anxiety, ways they handled it) Response to Failure on Test Items: Impulsivity: Ms. X has past history of at least one violent episode. During that incident patient beat one of her daughters with a telephone. This is an example of Ms. X exhibiting impulsivity. Anxiety: Distress after major life stressor have contributed to Ms. X’s depression and possible suicide attempt. Past conflicts with her daughters and some occupational conflicts with coworkers have added anxiety to the patient’s life.
Discharge Plans and Instruction: Placement, outpatient treatment, partial hospitalization, sober living, board and care, shelter, long term care facility, 12 step program
Teaching Assessment and Client / Family Education: (Disease process, medication, coping, relaxation, diet, exercise, hygiene) Include barriers to learning and preferred learning styles
Ms. X will remain in outpatient treatment. Client will continue to take Abilify 15 mg q day for treatment of Schizophrenia, Paranoid Type, goal is to diminished manifestations of this disorder positive symptoms which are delusions and hallucinations. In addition, Ms. X will continue on Prozac 20 q day which have antidepressant properties to help with major depressive episodes. Client will remain taking Klonopin 1 mg qhs for sleep to decreased anxiety associated with depression which will help to decrease agitation associated with psychotic symptoms. At this moment a diagnosis of Schizoaffective Disorder, Depressed Type is considered which might required mood stabilize therapy with lithium. Lithium is known to alter at least two intracellular second messenger systems,
Patient states that her daughters are her primary support system. Refer Ms. X and her daughters to family therapy which may help improving their relationship. In addition, family therapy will give Ms. X’s daughters improved insight to her mother’s illness and it will guide them on how to help her. Also, encouraging family activities like once a week game night will help increase patient’s social interactions. Provide medication side effects teaching to Ms. X’s daughters. In addition, advise Ms. X’s daughters that patient should not drink alcohol or caffeine due to many interactions with schizophrenia and other medications. Also, educate them about not arguing with the client’s delusions, instead focus on her feelings and offer reasonable explanations. Improvement of the patient’s primary
Course: NURS 223L PSYCHIATRIC NURSING CARE PLAN TEMPLATE and affecting norepinephrine and serotonin in the CNS. In addition to altering GABA metabolism and ion channel function. Lithium has many side effects and can become toxic even at prescribed therapeutic doses. Lithium risks may outweigh the benefits for this patient. Another mood stabilizer may need to be prescribed if patient does not remain stable. Ms. X will be educated on the importance of medication compliance. Considering that the client lives by herself and has a limited social life which increases her levels of anxiety and distress, especially since her youngest daughter moved out, it is needed to encourage patient to develop social skills and to increase social interactions. In addition, individual psychotherapy will help Ms. X remain out of depression. Continue to monitor patient’s general medical conditions and stabilize them in order to improve her prognosis cause her general medical conditions which include diabetes mellitus type 2 adult onset, hypertension, bilateral lumbar radiculopathy, back pain, bilateral knee pain, BPPV(benign paroxysmal positional vertigo, stress incontinence, and constipation) have been adding stress to her life. Patient has a good prognosis if her psychotic episodes are controlled and her severe depression stabilized. Ms. X’s life expectancy is expected to be similar to her peers.
Pertinent Lab Tests Results (normal ranges in parentheses) Valproic Acid (50 – 120 mcg/mL) Lithium (0.5 – 1.2 mEq/L) Carbamazepine (5 – 12 mcg/mL) CBC (WBC with diff, ANC, RBC) Urine Drug Screen Thyroid Panel Page 6 of 21
support system and social interactions will be important in maintaining continued health.
Rationale for Abnormals
N/A N/A N/A N/A N/A N/A
Course: NURS 223L PSYCHIATRIC NURSING CARE PLAN TEMPLATE
Liver Function (AST/ALT, LHD, Albumin, Bilirubin) Kidney Function (BUN, creatinine) CK-Total/Creatine Kinase, Total, Serum
Vitamin D, 25-Hydroxy/Vitamin D, 25-Hydr
N/A Results: 367 U/L Normal Ranges: 24-173 H Rationale: Creatine phosphokinase is an enzyme that is found on the heart, brain, and skeletal muscles that when organs break down it causes this amount to rise. In this patient the elevated levels of creatine phosphokinase are associated with the incidence of psychosis-associated creatine kinaseemia. Also, psychotic schizophrenic patients are shown to exhibit chronic episodes of psychosis showing increased levels of creatine phosphokinase. Allen, P. (2012, May). Creatine metabolism and psychiatric disorders: Does creatine supplementation have therapeutic value? Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3340488/ Results: 22.7 ng/mL Normal Ranges: 32.0-100.0 L Rationale: The 25-hydroxy vitamin D test monitors the amount of vitamin D levels in your blood which can indicates how much vitamin D the body has by determining if your vitamin D levels are too high or too low. Ms. X has a history of bone pain which is an indicator of vitamin D levels are too low. Wu, E. (2019, January 24). 25-Hydroxy Vitamin D Test: Purpose, Procedure, and Results. Retrieved from https://www.healthline.com/health/25-hydroxy-vitamin-d-test
Blood Alcohol Level Diagnostic Test Results (with dates) Physical Exam 6/11/08 Mammogram 6/11/08 Pap Smear 6/11/08 Urinalysis 6/11/08 CT Neuroimaging 4/30/09
N/A Rationale for Abnormals
Normal Normal Normal Normal Abnormal= Mild cerebral atrophy: Causes some changes in the structure of the brain. Cerebral atrophy denotes a decrease in brain size of the brain. “Brain atrophy refers to a loss of brain cells or a loss in the number of connections between brain cells. People who experience brain atrophy typically develop poorer cognitive functioning as a result of this type of brain damage”(Seunggu, 2020). Studies have shown that brain volume loss can be result from antipsychotic treatment in some schizophrenia patients. In Ms. X case this is the most accurate finding sustaining her abnormal result for mild cerebral atrophy (Antipsychotics and Brain Damage, 2016). Antipsychotics and Brain Damage (2016, September 24). Shrinkage & Volume Loss. Retrieved from https://mentalhealthdaily.com/2015/07/03/antipsychotics-and-brain-damage-shrinkagevolume-loss/
Page 7 of 21
Course: NURS 223L PSYCHIATRIC NURSING CARE PLAN TEMPLATE
Seunggu, H. (2020, January 8). Brain atrophy: Symptoms, causes, and outlook. Retrieved from https://www.medicalnewstoday.com/...
Similar Free PDFs

Mental Health Care Plan
- 8 Pages

Mental Health Clinical Care Plan
- 1 Pages

Mental Health SBAR Plan of Care
- 4 Pages

Uworld Mental Health Nursing
- 168 Pages

N101L Care Plan - Nursing Care Plan
- 11 Pages

Nursing-Care-Plan Example
- 12 Pages

Nursing Care Plan. 2
- 2 Pages

Care plan for nursing
- 1 Pages

Nursing Care Plan Activity
- 2 Pages

Nursing Care Plan- mobility
- 2 Pages

65209370 Nursing Care Plan
- 31 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu