Sandra Littlefield Care Plan PDF
| Title | Sandra Littlefield Care Plan |
|---|---|
| Author | Asia Anderson |
| Course | Nursing of Adults - Mental Health and Maladaptive Behavior |
| Institution | Oakland Community College |
| Pages | 12 |
| File Size | 369.6 KB |
| File Type | |
| Total Downloads | 34 |
| Total Views | 170 |
Summary
This is a care plan made from a Vsim from course point, Sandra Littlefield...
Description
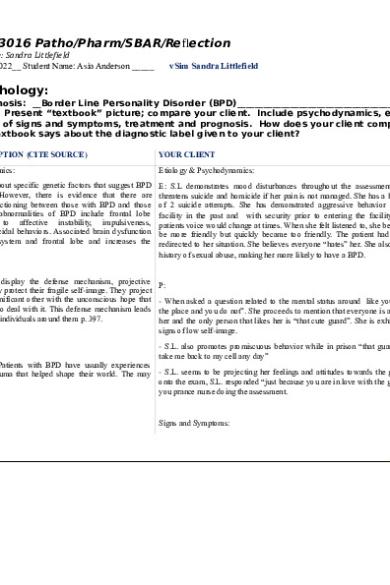
vSIM NRS 3016 Patho/Pharm/SBAR/Reflection Mental Health Case: Sandra Littlefield Date: January 21, 2022__ Student Name: Asia Anderson _____
vSim Sandra Littlefield
Psychopathology: Axis I Diagnosis: __Border Line Personality Disorder (BPD)_______________________________________ Directions: Present “textbook” picture; compare your client. Include psychodynamics, etiology, description of signs and symptoms, treatment and prognosis. How does your client compare with what the textbook says about the diagnostic label given to your client? TEXTBOOK DESCRIPTION (CITE SOURCE)
YOUR CLIENT
Etiology & Psychodynamics:
Etiology & Psychodynamics:
E: It remains unclear about specific genetic factors that suggest BPD traits are inheritable. However, there is evidence that there are differences in brain functioning between those with BPD and those without it. Biological abnormalities of BPD include frontal lobe dysfunction leading to affective instability, impulsiveness, aggressiveness, and suicidal behaviors. Associated brain dysfunction occurs in the limbic system and frontal lobe and increases the behaviors of p. 397.
E: S.L demonstrates mood disturbances throughout the assessment, She threatens suicide and homicide if her pain is not managed. She has a history of 2 suicide attempts. She has demonstrated aggressive behavior in the facility in the past and with security prior to entering the facility. The patients voice would change at times. When she felt listened to, she began to be more friendly but quickly became too friendly. The patient had to be redirected to her situation. She believes everyone “hates” her. She also has a history of sexual abuse, making her more likely to have a BPD.
P: Persons with BPD display the defense mechanism, projective identification where they protect their fragile self-image. They project their feelings onto a significant other with the unconscious hope that the person knows how to deal with it. This defense mechanism leads to more rejection by the individuals around them p. 397.
P: - When asked a question related to the mental status around like you own the place and you do not”. She proceeds to mention that everyone is against her and the only person that likes her is “that cute guard”. She is exhibiting signs of low self-image. - S.L. also promotes promiscuous behavior while in prison “that guard can take me back to my cell any day”
Signs and Symptoms: Patients with BPD have usually experiences significant losses or trauma that helped shape their world. The may - S.L. seems to be projecting her feelings and attitudes towards the guards onto the exam, S.L. responded “just because you are in love with the guards, display signs of: you prance nurse doing the assessment. - Inhibited grieving - Cognitive disturbances Signs and Symptoms:
- Identity disturbances (dissociation) - Transient psychotic episode, - Poor interpersonal skills - Low self-esteem and - Poor coping ability - Limited social support
- S.L. mentioned that she has been “through a lot” and has not learned proper techniques to grieve. - Throughout the assessment, S.L. displayed signs of impulsiveness when she would avoid answering a question and mention her pain. - S.L. works as a prostitute, which means that she is involved in impulsive risky behaviors. S.L. increases her risk of self-injury by having increasing numbers of sexual encounters. - S.L. also had cognitive disturbances, when asked a general question (unrelated to pain), she responded “you don’t really care about my pain”.
- Impulsiveness, - Parasuicide - Mood disturbances
- She reports that she feels alone and is afraid of being alone and possibly dying alone. She reports having no one to talk to, may be due to lack of interpersonal skills.
p. 401.
- She states “it’s not my fault that I’m in this place”, she is denying the situation that she (may have) caused. – Lack of coping - S.L. has had past suicide attempts
Treatment: Treatment: (Medications, Therapy, Other) - S.L. reports that she likes to read and listen to music. S.L. was encouraged - Treat the pain, give medication as prescribed and document the to visit the library or join support groups to cope. The nurse offered to escort findings S.L. to the library for support. - Identify if the patient is at risk of self-injury or suicide ideation and provide recovery goals alongside the patient. - Psychotherapy is advised and can include: o
dialectical behavior therapy
o
cognitive behavior therapy
- S.L. is encouraged to speak about her frustrations in a healthy setting and educated on ways to cope. - S.L. was encouraged to speak with a therapist in the facility and the nurse will provide community resources for her when she is released. - S.L. was provided alternative methods to relieve pain; ice packs, meditation, and exercise.
o
mentalization-based therapy
- Suicide Assessment
o
schema-focused therapy
- 24 hour surveillance
o
transference-focused psychotherapy
- Eating a well-balanced diet with a good eating pattern - Antidepressants (SSRI’s), mood stabilizers, antipsychotics, and antianxiety medication can be prescribed.
Prognosis: (Will it get better, stay the same, or get worse? Give your rationale for your prognosis) The condition will get better as long as the person follows up with individual therapy, psychoeducation, and positive environment. The patient would benefit from learning new coping techniques and Prognosis: healthy lifestyle patterns. Ms. Littlefield has been following up with therapy and reading in the library while in the facility. Ms. Littlefield has agreed to continue going to individual therapy after leaving the facility APA Style Reference:_ __ Boyd, M. A. (2019). Lippincott CoursePoint Enhanced for Boyd’s Essentials of Psychiatric Nursing (2nd ed.). Wolters Kluwer. __________________________ ______________________________________
PHARMACOLOGICAL AGENTS vSIM PHARM-4-FUN This activity provides you with the opportunity to create pertinent patient education on the pharmacological agents associated with the vSIM activity. You will utilize this worksheet for each drug listed under the pharmacology are of the suggested reading section.
Use one form/worksheet by color coding individual medications onto the form. vSIM Patient Medication Worksheet Medication (Generic & Brand) Name: Ibuprofen (Advil, Motrin)600 mg PO, BID Acetaminophen (Tylenol) 1000 mg PO, every 6 hours (qID)
Classification/Pharmacological Class: Antipyretics, Nonopioid analgesic, nonsteroidal anti-inflammatory drug (NSAID) Antipyretics, nonopioid analgesics Indication/Purpose for Taking This Medication: Treats pain and fever. Used to reduce pain, inflammation, and fever. Treats pain and fever with opioid analgesics Dosing range, Dosing Routes: PO: Anti-inflammatory - 400-800 mg 3-4 times daily (not to exceed 3200 mg/day) Analgesic/antipyretic – 200-400 mg every 4-6 hrs. (not to exceed 1200 mg/day) IV: Anti-inflammatory - 400-800 mg every 6 hrs. as needed (not to exceed 3200 mg/day) Analgesic/antipyretic –400 mg initially, then 400 mg every 4-6 hrs or 100-200 mg every 4 hrs as needed (not to exceed 3200 mg/day) PO: 325-650 mg every 6 hrs
1 g 3-4 times daily or 1300 mg every 8 hrs (not to exceed 3 g or 2 g/24 hr in patients with hepatic/renal impairment) IV: 1000 mg every 6 hrs or 650 mg every 4 hrs (not to exceed 1000 mg/dose, 4g/day [by all routes] and lrss than 4 hrs dosing interval)
Side Effects & Adverse Reactions: Headache, dizziness, drowsiness, intraventricular hemorrhage, psychic disturbances, heart failure, myocardial infarction, stroke, arrhythmias, edema, Steven-Johnson syndrome, GI bleeding, hepatitis, anemia, hypersensitivity reaction Steven -Johnson syndrome, toxic epidermal necrolysis, rash, hepatotoxicity, renal failure, neutropenia, pancytopenia Nursing Considerations: Patients with asthma, aspirin-induced allergy, and nasal polyps are at increased risk for developing hypersensitivity reactions. Assess for rhinitis, asthma, and urticaria Assess for s/s of GI bleeding (tarry stools, light-headedness, hypotension), renal dysfunction (elevated BUN and serum creatinine levels decreased urine output), and hepatic impairment (elevated liver enzymes, jaundice). Assess overall health status and alcohol usage before administering. Assess for rash periodically during therapy. If overdose occurs, acetylcysteine (Acetadote) is the antidote Patient Teaching: Advise patient to take ibuprofen with a full glass of water and take medication as directed. Caution patient to not take medicine with alcohol, aspirin, acetaminophen, or any OTC herbal medication. Advise patient to take medication exactly as directed and not to take more than recommended. Advise patient to avoid alcohol.
Mental Health Case: Sandra Littlefield Documentation Assignment 1. Document your findings related to the focused assessment of Ms. Littlefield's coping strategies. Include her responses to your assessment. Ms. Littlefield had pain but did not have pharmacologic interventions. She appeared frustrated, hopeless, and anxious. Ms. Littlefield shared that she enjoys reading and listening to music. The nurse offered to escort her to the library and shared coping techniques that she can use in the facility.
2. Document all patient teaching regarding coping strategies and cognitive restructuring techniques provided Ms. Littlefield. Include her response to the teaching. Coping: I stated, “There are several strategies you can utilize to decrease feelings of anxiety, frustration or fear. For example, community support groups and regular appointments with a therapist will help you to increase self awareness and reduce the potential for destructive acting out behaviors. While you are in prison, I can assist you with identifying community resources when you are released. Is there anything you have done in the past that has helped to reduce your anxiety or frustration”. Ms. Littlefield responded, “I have enjoyed taking walks and reading more romance novels”, I answered “Perhaps we can talk about some exercises you can do while in prison. There is a small library with books and magazines that is available to you here. We can walk there together.” Medications: I stated, “Ms. Littlefield, you have been prescribed two medications for pain. Both are over-the-counter medications that also reduce inflammation associated with pain. You may have two 500-mg tablets of acetaminophen every 6 hours, not to exceed 6 tablets per day or 3000-mg. You may also have ibuprofen, 600-mg, every 8 hours.” Pain management: I stated, “I would like to talk to you about other methods to relieve pain that don’t involve painkillers,” The patient replied, “I don’t think that will work, but what can I do”” I replied, “There are a number of interventions you could use, like applying ice packs, stretching exercises, and core strengthening, to name a few. I could should you when you are ready for that?”. 3. Referring to your feedback log, document all nursing care provided and Ms. Littlefield's response to this care. I began by checking the scene for safety before entering the room, introduce myself, washed my hands, identified the patient, completed vital signs. I assessed the patient’s attention, motor activity, speech, and thought processes. I asked the patient “Can you tell me a little bit more about what’s going on with you today?” she replied “I am in so much pain. You are a nurse. Don’t you know how to tell when someone is hurting?” I asked if she was feeling overwhelmed and she replied that she is. I asked if it would be alright to ask a series of questions to help start to plan her care, Ms. Littlefield replies “Just because you are in love with the guards, you prance around like you own this place and you do not!”, I attempted to therapeutically control the situating by saying, “Ms. Littlefield, you need to lower your voice now. I am here to help you.” I continued to use therapeutic ways of communication with Ms. Littlefield. Her mood began to change, she became calm, her posture changed, and she was more receptive to information. I asked her “ Can you tell me what a desired outcome of treatment would be for you?” She replied, “Everyone is against me. You, the other nurses, the provider…you all hate me. The only one who likes me is that cute guard.” I answered, “You feel that people hate you?”, She replied, “Yes, I feel so alone in here”. I redirected the conversation to focus on the patient and her treatment. I am also assessing the patients mental status; concentration, behavior, speech, etc..
4. Document all interventions associated with boundary and limit setting directed toward managing Ms. Littlefield's manipulative behavior. I asked Ms. Littlefield, “I would like to ask you a series of questions about how you are feeling to help me better understand how together we can start to plan your care. These are questions I ask all of the patients I see. May I ask you these questions?” She replied, “Just because you are in love with the guards, you prance around like you own this place and you do not!” I answered, “Ms. Littlefield, you need to lower your voice now. I am here to help you.” I used the therapeutic technique of giving information. I asked, “Have you had any changes in your appetite over the past month?” She replied, “When I was in my 20’s, all the men followed me around. You’re cute: I bet you get looks like that too” I answered “We are here to talk about you today”. I used the therapeutic technique of giving information and setting limits. 5. Document all of Ms. Littlefield's attempts at “splitting” and include interventions implemented to respond appropriately. I asked Ms. Littlefield, “Can you tell me what a desired outcome of treatment would be for you?” She replied, “Everyone is against me. You, the other nurses, the provider…you all hate me. The only one who likes me is that cute guard.” I answered, “You feel that people hate you?”, She replied, “Yes, I feel so alone in here”. I used the therapeutic technique of restating. I asked Ms. Littlefield, “How do you understand your problems?” She replied, “I love talking to you. I wish you were here all the time. You are my favorite nurse.” I answered, “Is there something besides your back pain you would like to talk about?” I used the therapeutic technique of broad openings.
6. Document your handoff report in the SBAR format to communicate Ms. Littlefield's future needs.
vSIM ISBAR ACTIVITY This ISBAR activity assists you in building the skill of communicating pertinent information when caring for a patient. Appropriate actions you should do to complete this activity include finding appropriate data to provide a thorough ISBAR report.
vSIM ISBAR ACTIVITY STUDENT WORKSHEET Sandra Littlefield
INTRODUCTION/IDENTIFICATION Identify your name, position
SITUATION/SUBJECT State patient’s name, age, reason for admission
BACKGROUND State patient’s primary diagnosis, past history of suicidal or self-harm behaviors, allergies, current orders.
ASSESSMENT
Hello, my name is Asia. I will be your nurse today while you are at _____ Corrections facility.
Sandra Littlefield is a 36 year old female, she has been in jail for one week on prostitution charges. She has complained of back pain for which she was given ibuprofen 600 mg PO, BID and acetaminophen 1000 mg PO, every 6 hours (qID)
Ms. Littlefield has been diagnosed with borderline personality disorder. She has been incarcerated in the past and has been aggressive during past incarcerations. She has a history of sexual abuse, suicide attempts, drug and alcohol problems. She frequently visits the ER for back pain asking for stronger medications as ibuprofen and acetaminophen do not relieve her pain.
BP: 132/80, HR: 84, RR: 16, Temp: 98.6F, SPO2: 98,
State significant finding of this shift’s bio-psychosocial assessment (include self-harm/other harm, change in functioning, appetite, sleep, ability to complete ADLs, and noted psychosis), pertinent diagnostics (labs, procedures, etc.), vital signs, any PRN medications given during the shift and outcome.
Height: 172cm, Weight: 63kg We performed a mental status exam today that avoided asking too many questions about physical complaints from the patient. Ms. Littlefield is appropriately dressed with good personal hygiene. She was able to focus, demonstrated good insight, and goal directed thought. She did not have any inappropriate movements. She had poor personal boundaries between herself and staff. She expressed pain at a level of 8 in her back that was not managed with Tylenol. She expressed that she was not interested in any nonpharmacological interventions for her pain. She displayed frustration and anxiety in her speech. She had scars on her wrist from self-harm
RECOMMENDATION State any recommendations, nursing interventions, or orders that may need to be addressed.
- It is recommended that Ms. Littlefield be encouraged to try different nonpharmacological interventions for her pain. She should also be provided with access and information regarding addiction treatment services. Her pain levels should be monitored and administer analgesics as they are prescribed and as she asks for them
Student Reflection Questions: Opening Questions 1. How did the simulated experience of Sandra Littlefield's case make you feel?
Based off of my first observations of the patient, I thought she looked mean and seemed very intense. I had to check my bias and continue assessing her. As I talked to her more, I noticed that she became more comfortable with me as a nurse but had periods where she would get too comfortable. I learned proper therapeutic techniques to redirect her and refocus the interview on her.
2. Talk about what went well in the scenario. I think I did a good job providing therapeutic responses to Ms. Littlefield. I was able to get enough information to create a plan of care and to correctly complete the Mental Health Assessment. 3. Reflecting on Sandra Littlefield's case, were there any actions you would do differently? If so, what were these actions and why? I would have liked to provide more follow-up to some of the responses Ms. Littlefield had. Since it was a simulation, the answers were preselected which did not give me the opportunity to communicate with the patient like I would in real life. Scenario Analysis Questions* 1. PCC/S What should be the nurse's priority when caring for Sandra Littlefield? What action should be initiated to maintain personal safety? If the nurse did not recognize the importance of personal safety, what could be the consequence? The nurse needs to make sure it is a safe situation before entering the room. Make sure Ms. Littlefield is not suicidal or at risk of harming others. The nurse should maintain a safe distance from the patient. If the importance of safety is not recognized, the nurse can be harmed or hurt. 2. PCC/S
Discuss the importance of therapeutic communication and setting limits for Sandra Littlefield.
It is important to set limits for people with borderline personality disorder because they usually have poor personal boundaries and try to have inappropriate conversations with staff members. It is important to redirect the patient and refocus them on their treatment. If limits are not set, the patient will understand that there are boundaries and rules. 3. T&C/S
What members of the healthcare team should be involved in Sandra Littlefield's case?
The provider, a therapist, and a nurse should all be involved in Ms. Littlefield’s case.
Concluding Questions 1. Describe how you would apply the knowledge and skills that you obtained in Sandra Littlefield's case to an actual patient care situati...
Similar Free PDFs

Sandra Littlefield Care Plan
- 12 Pages

Sandra littlefield concept map
- 2 Pages

UTI Care Plan - Care Plan
- 7 Pages

Care plan 3 - Care Plan
- 3 Pages

Care Plan 1 - Care plan
- 7 Pages

Care Plan 2 - Care plan
- 21 Pages

N101L Care Plan - Nursing Care Plan
- 11 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu








