TEST 3 - test 3 review PDF
| Title | TEST 3 - test 3 review |
|---|---|
| Course | foundations of humanistic nursing practice |
| Institution | Molloy College |
| Pages | 19 |
| File Size | 988.9 KB |
| File Type | |
| Total Downloads | 68 |
| Total Views | 173 |
Summary
test 3 review ...
Description
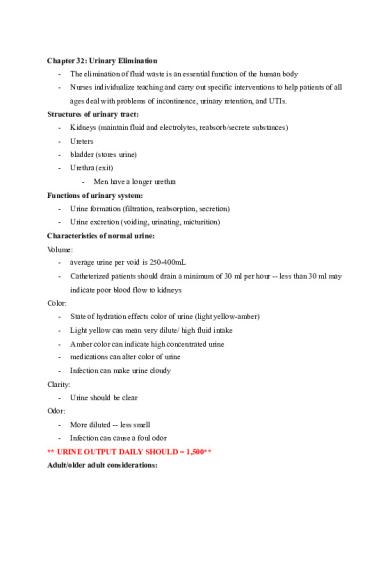
Chapter 32: Urinary Elimination -
The elimination of fluid waste is an essential function of the human body
-
Nurses individualize teaching and carry out specific interventions to help patients of all ages deal with problems of incontinence, urinary retention, and UTIs.
Structures of urinary tract: -
Kidneys (maintain fluid and electrolytes, reabsorb/secrete substances)
-
Ureters
-
bladder (stores urine)
-
Urethra (exit) -
Men have a longer urethra
Functions of urinary system: -
Urine formation (filtration, reabsorption, secretion)
-
Urine excretion (voiding, urinating, micturition)
Characteristics of normal urine: Volume: -
average urine per void is 250-400mL
-
Catheterized patients should drain a minimum of 30 ml per hour -- less than 30 ml may indicate poor blood flow to kidneys
Color: -
State of hydration effects color of urine (light yellow-amber)
-
Light yellow can mean very dilute/ high fluid intake
-
Amber color can indicate high concentrated urine
-
medications can alter color of urine
-
Infection can make urine cloudy
Clarity: -
Urine should be clear
Odor: -
More diluted -- less smell
-
Infection can cause a foul odor
** URINE OUTPUT DAILY SHOULD = 1,500** Adult/older adult considerations:
-
Incontinence (involuntary loss of urine from bladder)
-
Men may experience altered urinary elimination related to prostatic hypertrophy and women may experience altered urinary elimination related to weakened perineal muscles
-
Urgency
-
Retention (inability to empty bladder)
-
Nocturia
Fluid intake, loss of body fluid, body position, cognition, and psychological issues can affect urinary patterns. Many other factors can predispose a person to disruptions of normal patterns of urinary elimination. Obstruction of urine flow, UTIs, hypotension, neurologic injury, decreased muscle tone, pregnancy, surgery and medication are common causes. Altered urinary function: -
dysuria(painful)
-
Polyuria (increase urine)
-
Oliguria (decreased urine)
-
Anuria (no urine)
-
Urgency (being unable to delay voiding)
-
Frequency (voiding more than normal)
-
Nocturia (urinating during sleeping hours)
-
Hematuria (blood in urine)
-
Pyuria (pus in urine)
Types of incontinence: Stress incontinence: -
sudden, involuntary loss of small amounts of urine ex. Jumping rope, laughing
-
Causes: Weak pelvic floor, obesity, pregnancy
Urge incontinence: -
overactive bladder
-
Caused by overactive detrusor muscles
Overflow incontinence: -
Most likely men with enlarged prostates
-
Frequent urination of small amounts
Reflex incontinence:
-
unable to sense full bladder due to neurological impairment
Functional incontinence: -
Inability or unwillingness of a person with a normal bladder and sphincter control to reach the bathroom in time to void
Total incontinence: -
Continuous, involuntary,unpredictable loss of urine from a non distended bladder
Assessment of GU Subjective: -
History of any UTI? Burning or pain when urinating?
-
recent/current problems
Objective: -
Assessment of urine
-
intake/output
-
Physical assessment -
Inspection (bladder will only be seen if has over 500ml in it)
-
Percussion
-
Palpation - start at the level of the umbilicus and move in a downward direction toward the pubic symphysis to detect distension
Diagnostic Tests: -
Random specimen: used when sterile technique is not required ex. Physical testing urine
-
Clean-catch or midstream specimen: free of microorganisms
-
24 hour specimen: used for an accurate measurement of kidney excretion of substances (urine protein, creatine, uric acid)
-
Specimen from catheter: maintain strict asepsis, catheter is placed long enough to get specimen. If patient already has a catheter a syringe is used to draw urine from sealing port
-
Urinalysis: provides data about the color, turbidity, pH, and specific gravity of urine and detects protein, glucose, ketones, RBC, WBC, bacteria or casts. 20-30ml , throw out first void
Urinary Catheterization: -
Straight cath is temporary (insert in and get urine and remove)
-
Indwelling is used for a longer period of time
Indwelling catheters are used for: -
Monitoring critically ill /acutely ill patients when accurate assessment of urinary output is needed
-
Management of terminally/severely ill patient
-
Urinary retention not manageable by intermittent catheterization or other means
-
Management of urinary incontinence in patients with stage 3 or 4 pressure ulcers on the trunk
**NEVER USED ON INCONTIENT PATIENTS-- HIGH RISK OF UTI. ONLY ON HOSPICE PT** -
Do not take urine specimen from bag -- use syringe to take from tubing
Chapter 33: Bowel Elimination -
The major nursing responsibilities associated with bowel elimination include assessing bowel function, promoting normal bowel health and intervening to manage alterations in bowel function.
Function of the intestine: -
Motility -
Segmentation: slows passage of intestinal contents to permit more complete digestion and absorption of nutrients
-
Peristalsis: propels intestinal contents
-
Absorption: large intestines
-
Defecation
-
Normal feces is 75% water, 25% waste
Life span considerations of adult/older adult: -
Gastrointestinal motility slows = constipation
-
Bowel movement decreases
-
Increase fluids and high-fiber foods
-
Esophageal emptying is delayed = aspiration risk
** a fluid intake of 2,000ml per day is necessary to meet cellular needs and have enough left over to promote soft stool consistency. When the body needs to conserve fluid, it will absorb water from the large intestine to meet needs**
Fecal diversions: -
The portion of intestine brought through the abdominal wall is known as a stoma
-
A segment of the large colon out to the abdominal skin is called a colostomy, portion of the ileum is used to make a stoma of the abdomen known as a ileostomy
Stoma assessment: -
Nurse should assess stoma for color and position (ideally should be a healthy pink)
-
Ostomy pouch should be emptied when ¼ or ⅓ full
-
The nurse or patient should cleanse skin around stoma and dry before applying a new ostomy pouch
-
The stoma must be measured accurately for an appliance of correctly sized opening to obtain proper fit
Assessment: -
Inspection -
Normally abdomen is convex
-
Hollow or scaphoid can be associated with malnutrition
-
Protuberant or distended can be associated with obesity, pregnancy, or accumulation of gas
-
Auscultate -
Bowel sounds in all quadrants every 5-15secs
-
Hypoactive = every 15-30secs
-
hyperactive= >5secs -
-
-
Borborygmus is stomach growling (not normal finding)
-
Absent bowel sounds = no sound in 1-2 min -- listen for 5 mins to determine
-
If patient has pain, auscultate quadrant last
-
No sounds for 72 hrs = paralytic ileus
Percussion -
Hollow tympany in LUQ (stomach- contains more air)
-
Dull, tympany in quadrants other than LUQ are abnormal
Palpate -
Not done if pain in stomach
Enemas: cleanses a portion of the large bowel by inserting fluid rectally -
Small volume enemas: hypertonic, 150 ml
-
Large volume enemas: distended bowel with 750-1000 ml of fluid -- used to cleanse bowel
** hold as long as pt can (½ hr to 1 hr) -
return flow enema: relieves gas
Aortic aneurysm- bruit, vascular sound DO NOT PALPATE
Chapter 23: Neurologic System The nervous system can be divided into two parts: -
Central nervous system (CNS) includes brain and spinal cord
-
Peripheral nervous system includes all nerve fibers outside the brain and spinal cord (12 cranial nerves and 31 pairs of spinal nerves)
CNS: -
Cerebral cortex is the center of the highest functions (memory, reasoning, thought, sensation)
-
Each hemisphere has 4 lobes: -
Frontal (personality, behavior, emotion)
-
Parietal (sensation)
-
Occipital (visual receptor center)
-
Temporal (hearing, taste, smell)
-
Wernickie’s area (language comprehension -- patients with damage to area have receptive aphasia meaning they can hear sounds but it has no meaning to them)
-
broca ‘s area (motor speech -- patient with damage to area cannot talk but can put together what they want to say)
Hypothalamus- major respiratory center with basic vital functions: temperature, apetite, sex drive, heart rate, BP, sleep center, anterior/posterior pituatary gland regulator, and cordinator of ANS activity and stress response Sensory pathway- monitor conscious sensation, internal organ functions, body position and reflexes Motor pathway- mediate voluntary movement ex. Writing with a pen Reflex arc- basic defense mechanisms of the nervous system ex. Deep tendon reflex = knee jerk , visceral = pupillary light response and accomodation
Testing cranial nerves: CN I: Olfactory nerve -
Do not test routinely
-
Test on those who report loss of smell, head trauma, abnormal mental status
-
Test one nostril at a time and wave a familiar scent ex. Vanilla, coffee
CN II: Optic nerve -
Tests visual acuity and visual fields by confrontation tests
CN III,IV,VI: (3,4,6 eyes do tricks): oculomotor, trochlear, abducens nerves -
Check pupil size, regularity, equality, direct and consensual light reaction and accommodation
-
Check for any eye jerks or uncontrolled movements
CN V: trigeminal nerve -
Assess muscles of mastication
-
Test light touch sensation to test ophthalmic, maxillary and mandibular
CN VII: facial nerve -
Note mobility and facial symmetry as the person smiles
CN VIII: acoustic nerve -
Whisper voice test
CN IX, X: glossopharyngeal and vagus nerves -
Depress tongue and make patient say ahh
-
Gag reflex
CN XI: spinal accessory nerve -
Test resistance of shoulders, head and neck
CN XII: hypoglossal nerve -
Inspect tongue
-
Make patient say “light, tight, dynamite”
Testing cerebellar functions: -
Check for tics, tremors, myoclonus (muscle jerk), chorea (seizure like) , athetosis (cerebral palsy)
-
Finger to finger test
-
Finger to nose test
-
Heel to shin test
-
Observe a person's gait (walk 10-20 feet) -
-
Ataxia is uncoordinated or unsteady gait
Romberg test (balance test)
Spinothalamic tract: -
Pain: person's ability to perceive a pin prick
-
Light touch: apply cotton ball to skin
-
Vibration: ability to feel vibrations of a tuning fork over bony prominence
-
Graphesthesia: ability to read # by having it traced on skin
Test the reflexes:
4+ very brisk, hyperactive with clonus = disease 3+ brisker than average, may indicate disease 2+ average, normal 1+ diminished, low normal 0 no response Clonus- set of rapid, rhythmic contractions of the same muscle Hyperreflexia- exaggerated reflex ex. Stroke Hyporeflexia- absence of reflex ex. Spinal cord injury Paralysis- decreased or loss of motor power caused by problem with motor nerve or muscle fibers Paresis- weakness of muscles
Glascow coma scale- standardized, objective assessment that defines the level of consciousness by giving it a numeric value
Chapter 13: Head, Face, Neck, Regional Lymphatics
-
To palpate lymph nodes, use a gentle circular motion of your finger pads. Palpate with both hands, comparing each side.
-
Palapte these 10 locations:
-
When lymph nodes are enlarged, check the area they drain for the source of the problem -- explore area proximal to enlarged node
-
-
Head should feel symmetric and smooth, no tenderness to palpation -
microcephaly (small head)
-
Macrocephaly (large head)
During a head exam assess the following cranial nerves: -
CN V(trigeminal) for face strength and sensation
-
CN VII (facial) assess for symmetrical facial movement
-
CN XI (spinal accessory) head and shoulder strength
-
Temporal area should have a smooth movement when pt opens jaw
-
Note is facial expression is appropriate
-
Note any limitations of movement of the neck, test muscle strength of head/neck
-
Trachea is midline, palpate for any tracheal shift
-
Accommodation is adaption of the eye for near vision
-
Age related macular degeneration is a loss of central vision by yellow deposits
-
Presbyopia occurs by age 40 (age related vision loss)
-
Snellen- commonly used, accurate measure of visual acuity
-
Confrontation test- screens for loss of peripheral vision
-
Accommodation test is done by asking the person to focus on a distant object
-
Conductive hearing loss involves a mechanical dysfunction of the external or middle ear. It is a partial loss because the person is able to hear if the sound is increased to reach the inner ear. Can be caused by a foreign object, otosclerosis, buildup of earwax, etc.
-
Presbycusis is a gradual hearing loss over years
-
Weber test -
-
Normal results= sound is equally loud in both ears; does not lateralize
Rinne test -
Normal results = sound is heard twice as long by air conduction as by bone conduction is a positive Rinne test
adult - pinna pulled up and back Child- pinna pulled down and back...
Similar Free PDFs

TEST 3 - test 3 review
- 19 Pages

MCBL Test 3 - Review for test 3
- 6 Pages

Test 3 Review
- 2 Pages

Test 3 - Review
- 2 Pages

Test 3 Review
- 8 Pages

Review Test 3
- 2 Pages

MPO Test 3 Review
- 9 Pages

Test 3 Review Questions
- 7 Pages

IBF Test 3 - Test 3
- 1 Pages

Test 3 review - Prof. Mowsh
- 15 Pages
Human geography test 3 review
- 10 Pages

Unit 3 Psychology Test Review
- 5 Pages

Philosphy 150 test review 3
- 3 Pages

Yates Test 3 - Test
- 7 Pages

Abnormal Review for Test #3
- 6 Pages

Test leccion 3 - Test
- 3 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu