WHO Comprehensive Mental Health Action Plan 2013-2020 PDF

| Title | WHO Comprehensive Mental Health Action Plan 2013-2020 |
|---|---|
| Author | Ailene Alea |
| Course | Research Practicum |
| Institution | Eastern Visayas State University |
| Pages | 27 |
| File Size | 758.6 KB |
| File Type | |
| Total Downloads | 82 |
| Total Views | 506 |
Summary
WHO Comprehensive Mental Health Action Plan 2013-2020...
Description
SIXTY-SIXTH WORLD HEALTH ASSEMBLY Agenda item 13.3
WHA66.8 27 May 2013
Comprehensive mental health action plan 2013–2020 The Sixty-sixth World Health Assembly, Having considered the report by the Secretariat on the draft comprehensive action plan 2013‒2020, including the Annex,1 1.
ADOPTS the comprehensive mental health action plan 2013–2020;
2. URGES Member States to implement the proposed actions for Member States in the comprehensive mental health action plan 2013–2020 as adapted to national priorities and specific national circumstances; 3. INVITES international, regional and national partners to take note of the comprehensive mental health action plan 2013–2020; 4. REQUESTS the Director-General to implement the actions for the Secretariat in the comprehensive mental health action plan 2013–2020 and to submit reports on the progress achieved in implementing the action plan, through the Executive Board, to the Sixty-eighth, Seventy-first and Seventy-fourth World Health Assemblies.
1
Document A66/10 Rev.1.
WHA66.8
ANNEX COMPREHENSIVE MENTAL HEALTH ACTION PLAN 2013–2020 1. In May 2012, the Sixty-fifth World Health Assembly adopted resolution WHA65.4 on the global burden of mental disorders and the need for a comprehensive, coordinated response from health and social sectors at the country level. It requested the Director-General, inter alia, to develop a comprehensive mental health action plan, in consultation with Member States, covering services, policies, legislation, plans, strategies and programmes. 2. This comprehensive action plan has been elaborated through consultations with Member States, civil society and international partners. It takes a comprehensive and multisectoral approach, through coordinated services from the health and social sectors, with an emphasis on promotion, prevention, treatment, rehabilitation, care and recovery. It also sets out clear actions for Member States, the Secretariat and international, regional and national level partners, and proposes key indicators and targets that can be used to evaluate levels of implementation, progress and impact. The action plan has, at its core, the globally accepted principle that there is “no health without mental health”.1 3. The action plan has close conceptual and strategic links to other global action plans and strategies endorsed by the Health Assembly, including the global strategy to reduce the harmful use of alcohol, the global plan of action for workers’ health, 2008–2017, the action plan for the global strategy for the prevention and control of noncommunicable diseases, 2008–2013, and the global action plan for the prevention and control of noncommunicable diseases (2013–2020). It also draws on WHO’s regional action plans and strategies for mental health and substance abuse that have been adopted or are being developed. The action plan has been designed to create synergy with other relevant programmes of organizations in the United Nations system, United Nations interagency groups and intergovernmental organizations. 4. The action plan builds upon, but does not duplicate, the work of WHO’s mental health gap action programme (mhGAP). The focus of the latter was to expand services for mental health in low-resource settings. The action plan is global in its scope and is designed to provide guidance for national action plans. It addresses, for all resource settings, the response of social and other relevant sectors, as well as promotion and prevention strategies. 5. In this action plan, the term “mental disorders” is used to denote a range of mental and behavioural disorders that fall within the International Statistical Classification of Diseases and Related Health Problems (Tenth revision). These include disorders that cause a high burden of disease such as depression, bipolar affective disorder, schizophrenia, anxiety disorders, dementia, substance use disorders, intellectual disabilities, and developmental and behavioural disorders with onset usually occurring in childhood and adolescence, including autism. For dementia and substance use disorders, additional prevention strategies may also be required (as, for example, described in a WHO report on dementia issued in early 20122 and the global strategy to reduce the harmful use of alcohol). 1 See the WHO web site (http://www.who.int/mental_health/mhgap/consultation_global_mh_action_plan_ 2013_2020/en/index.html) for: a glossary of main terms; links to other global action plans, strategies and programmes; international and regional human rights treaties; and selected WHO technical materials and resources on mental health. 2
2
WHO, Alzheimer’s Disease International. Dementia: a public health problem. Geneva, World Health Organization, 2012.
Annex
WHA66.8
Furthermore, the plan covers suicide prevention and many of the actions are also relevant to conditions such as epilepsy. The term “vulnerable groups” is used in the action plan to refer to individuals or groups of individuals who are made vulnerable by the situations and environments that they are exposed to (as opposed to any inherent weakness or lack of capacity). The term “vulnerable groups” should be applied within countries as appropriate to the national situation. 6. The action plan also covers mental health, which is conceptualized as a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community. With respect to children, an emphasis is placed on the developmental aspects, for instance, having a positive sense of identity, the ability to manage thoughts, emotions, and to build social relationships, as well as the aptitude to learn and acquire an education, ultimately enabling their full active participation in society. 7. In light of the widespread human rights violations and discrimination experienced by people with mental disorders, a human rights perspective is essential in responding to the global burden of mental disorders. The action plan emphasizes the need for services, policies, legislation, plans, strategies and programmes to protect, promote and respect the rights of persons with mental disorders in line with the International Covenant on Civil and Political Rights, the International Covenant on Economic, Social and Cultural Rights, the Convention on the Rights of Persons with Disabilities, the Convention on the Rights of the Child and other relevant international and regional human rights instruments.
OVERVIEW OF THE GLOBAL SITUATION 8. Mental health is an integral part of health and well-being, as reflected in the definition of health in the Constitution of the World Health Organization: “health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”. Mental health, like other aspects of health, can be impacted by a range of socioeconomic factors (described below) that need to be addressed through comprehensive strategies for promotion, prevention, treatment and recovery in a whole-ofgovernment approach.
Mental health and disorders: determinants and consequences 9. Determinants of mental health and mental disorders include not only individual attributes such as the ability to manage one’s thoughts, emotions, behaviours and interactions with others, but also social, cultural, economic, political and environmental factors such as national policies, social protection, living standards, working conditions, and community social supports. Exposure to adversity at a young age is an established preventable risk factor for mental disorders. 10. Depending on the local context, certain individuals and groups in society may be placed at a significantly higher risk of experiencing mental health problems. These vulnerable groups may (but not necessarily) include members of households living in poverty, people with chronic health conditions, infants and children exposed to maltreatment and neglect, adolescents first exposed to substance use, minority groups, indigenous populations, older people, people experiencing discrimination and human rights violations, lesbian, gay, bisexual, and transgender persons, prisoners, and people exposed to conflict, natural disasters or other humanitarian emergencies. The current global financial crisis provides a powerful example of a macroeconomic factor leading to cuts in funding despite a concomitant need for more mental health and social services because of higher rates of mental disorders and suicide as well as the emergence of new vulnerable groups (for example, the young unemployed). In many societies, mental disorders related to marginalization and
3
WHA66.8
Annex
impoverishment, domestic violence and abuse, and overwork and stress are of growing concern, especially for women’s health. 11. People with mental disorders experience disproportionately higher rates of disability and mortality. For example, persons with major depression and schizophrenia have a 40% to 60% greater chance of dying prematurely than the general population, owing to physical health problems that are often left unattended (such as cancers, cardiovascular diseases, diabetes and HIV infection) and suicide. Suicide is the second most common cause of death among young people worldwide. 12. Mental disorders often affect, and are affected by, other diseases such as cancer, cardiovascular disease and HIV infection/AIDS, and as such require common services and resource mobilization efforts. For example, there is evidence that depression predisposes people to myocardial infarction and diabetes, both of which conversely increase the likelihood of depression. Many risk factors such as low socioeconomic status, alcohol use and stress are common to both mental disorders and other noncommunicable diseases. There is also substantial concurrence of mental disorders and substance use disorders. Taken together, mental, neurological and substance use disorders exact a high toll, accounting for 13% of the total global burden of disease in the year 2004. Depression alone accounts for 4.3% of the global burden of disease and is among the largest single causes of disability worldwide (11% of all years lived with disability globally), particularly for women. The economic consequences of these health losses are equally large: a recent study estimated that the cumulative global impact of mental disorders in terms of lost economic output will amount to US$ 16.3 million between 2011 and 2030.1 13. Mental disorders frequently lead individuals and families into poverty.2 Homelessness and inappropriate incarceration are far more common for people with mental disorders than for the general population, and exacerbate their marginalization and vulnerability. Because of stigmatization and discrimination, persons with mental disorders often have their human rights violated and many are denied economic, social and cultural rights, with restrictions on the rights to work and education, as well as reproductive rights and the right to the highest attainable standard of health. They may also be subject to unhygienic and inhuman living conditions, physical and sexual abuse, neglect, and harmful and degrading treatment practices in health facilities. They are often denied civil and political rights such as the right to marry and found a family, personal liberty, the right to vote and to participate effectively and fully in public life, and the right to exercise their legal capacity on other issues affecting them, including their treatment and care. As such, persons with mental disorders often live in vulnerable situations and may be excluded and marginalized from society, which constitutes a significant impediment to the achievement of national and international development goals. The Convention on the Rights of Persons with Disabilities, which is binding on States Parties that have ratified or acceded to it, protects and promotes the rights of all persons with disabilities, including persons with mental and intellectual impairments, and also promotes their full inclusion in international cooperation including international development programmes.
Health system resources and responses 14. Health systems have not yet adequately responded to the burden of mental disorders; as a consequence, the gap between the need for treatment and its provision is large all over the world. 1 World Economic Forum, the Harvard School of Public Health. The global economic burden of non-communicable diseases. Geneva, World Economic Forum, 2011. 2
Mental health and development: targeting people with mental health conditions as a vulnerable group. Geneva, World Health Organization, 2010.
4
Annex
WHA66.8
Between 76% and 85% of people with severe mental disorders receive no treatment for their disorder in low-income and middle-income countries; the corresponding range for high-income countries is also high: between 35% and 50%. A further compounding problem is the poor quality of care for those receiving treatment. WHO’s Mental Health Atlas 2011 provides data that demonstrate the scarcity of resources within countries to meet mental health needs, and underlines the inequitable distribution and inefficient use of such resources. Globally, for instance, annual spending on mental health is less than US$ 2 per person and less than US$ 0.25 per person in low-income countries, with 67% of these financial resources allocated to stand-alone mental hospitals, despite their association with poor health outcomes and human rights violations. Redirecting this funding towards community-based services, including the integration of mental health into general health care settings, and through maternal, sexual, reproductive and child health, HIV/AIDS and chronic noncommunicable disease programmes, would allow access to better and more cost-effective interventions for many more people. 15. The number of specialized and general health workers dealing with mental health in low-income and middle-income countries is grossly insufficient. Almost half the world’s population lives in countries where, on average, there is one psychiatrist to serve 200 000 or more people; other mental health care providers who are trained in the use of psychosocial interventions are even scarcer. Similarly, a much higher proportion of high-income countries than low-income countries reports having a policy, plan and legislation on mental health; for instance, only 36% of people living in low-income countries are covered by mental health legislation compared with 92% in high-income countries. 16. Civil society movements for mental health in low-income and middle-income countries are not well developed. Organizations of people with mental disorders and psychosocial disabilities are present in only 49% of low-income countries compared with 83% of high-income countries; for family associations the respective figures are 39% and 80%. 17. Finally, the availability of basic medicines for mental disorders in primary health care is notably low (in comparison to medicines available for infectious diseases and even other noncommunicable diseases), and their use restricted because of the lack of qualified health workers with the appropriate authority to prescribe medications. In addition, the availability of non-pharmacological approaches and trained personnel to deliver these interventions is also lacking. Such factors act as important barriers to appropriate care for many persons with mental disorders. 18. To improve the situation, and in addition to the data on mental health resources in countries (from WHO’s Mental Health Atlas 2011, as well as the more detailed profiling obtained through use of WHO’s Assessment Instrument for Mental Health Systems),1 information is available on costeffective and feasible mental health interventions that can be expanded to a larger scale to strengthen mental health care systems in countries. WHO’s Mental Health Gap Action Programme, launched in 2008, uses evidence-based technical guidance, tools and training packages to expand service provision in countries, especially in resource-poor settings. It focuses on a prioritized set of conditions and, importantly, directs its capacity building towards non-specialized health care providers in an integrated approach that promotes mental health at all levels of care. 19. The Secretariat has elaborated other technical tools and guidance in support of countries in developing comprehensive mental health policies, plans and laws that promote improved quality and availability of mental health care (such as the WHO mental health policy and service guidance
1
WHO-AIMS version 2.2: World Health Organization Assessment Instrument for Mental Health Systems, Geneva, World Health Organization, 2005 (document WHO/MSD/MER/05.2).
5
WHA66.8
Annex
package);1 in improving quality and respecting the rights of persons with mental disorders in health services (the WHO QualityRights toolkit);2 and for disaster relief and post-disaster mental health system reconstruction (including the Inter-Agency Standing Committee Guidelines in mental health and psychosocial support in emergency settings).3 Knowledge, information and technical tools are necessary but not sufficient; strong leadership, enhanced partnerships and the commitment of resources towards implementation are also required in order to move decisively from evidence to action and evaluation.
STRUCTURE OF THE COMPREHENSIVE ACTION PLAN 2013–2020 20. The vision of the action plan is a world in which mental health is valued, promoted and protected, mental disorders are prevented and persons affected by these disorders are able to exercise the full range of human rights and to access high quality, culturally-appropriate health and social care in a timely way to promote recovery, all in order to attain the highest possible level of health and participate fully in society and at work free from stigmatization and discrimination. 21. Its overall goal is to promote mental well-being, prevent mental disorders, provide care, enhance recovery, promote human rights and reduce the mortality, morbidity and disability for persons with mental disorders. 22.
The action plan has the following objectives: (1)
to strengthen effective leadership and governance for mental health;
(2) to provide comprehensive, integrated and responsive mental health and social care services in community-based settings; (3)
to implement strategies for promotion and prevention in mental health;
(4)
to strengthen information systems, evidence and research for mental health.
The global targets established for each objective provide the basis for measurable collective action and achievement by Member States towards global goals and should not negate the setting of more ambitious national targets, particularly for those countries that have already reached global ones. Indicators for measuring progress towards defined global targets are provided in Appendix 1. 23.
The action plan relies on six cross-cutting principles and approaches: • Universal health coverage: Regardless of age, sex, socioeconomic status, race, ethnicity or sexual orientation, and following the principle of equity, persons with mental disorders should be able to access, without the risk of impoverishing themselves, essential health and social services that enable them to achieve recovery and the highest attainable standard of health.
1
http://www.who.int/mental_health/policy/essentialpackage1/en/index.html (accessed 24 May 2013).
2
WHO QualityRights tool kit: assessing and improving quality and human rights in mental health and social care facilities. Geneva, World Health Organization, 2012. 3 Inter-Agency Standing Committee. IASC guidelines on mental health and psychosocial support in emergency setting...
Similar Free PDFs

Mental Health Gap Action
- 5 Pages

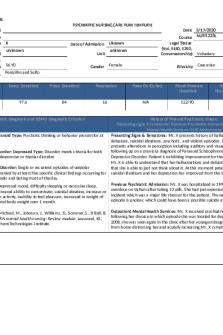
Mental Health Care Plan
- 8 Pages

Mental Health Clinical Care Plan
- 1 Pages

Mental Health SBAR Plan of Care
- 4 Pages

Mental Health
- 44 Pages

ACTION PLAN-FEEDING
- 2 Pages

ACTION PLAN IN ENGLISH
- 4 Pages

ACTION PLAN IN SCIENCE
- 4 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu