Wilkins Lippinco 2016 15Drugs For Fluid And Ele Pharmacology Made Incre PDF

| Title | Wilkins Lippinco 2016 15Drugs For Fluid And Ele Pharmacology Made Incre |
|---|---|
| Course | Current Issues-Nurs |
| Institution | Ohio University |
| Pages | 23 |
| File Size | 945.2 KB |
| File Type | |
| Total Downloads | 34 |
| Total Views | 145 |
Summary
Download Wilkins Lippinco 2016 15Drugs For Fluid And Ele Pharmacology Made Incre PDF
Description
Chapter 15
Drugs for fluid and electrolyte balance
opyright 2016. Wolters Kluwer Health. ll rights reserved. May not be reproduced in any form without permission from the publisher, except fair uses permitted under U.S. or applicable copyright law.
Just the facts In this chapter, you’ll learn: classes of drugs used to treat fluid and electrolyte disorders uses and varying actions of these drugs absorption, distribution, metabolization, and excretion of these drugs drug interactions and adverse reactions to these drugs.
Drugs and homeostasis Illness can easily disturb the homeostatic mechanisms that help maintain normal fluid and electrolyte balance. Such occurrences as loss of appetite, medication administration, vomiting, surgery, and diagnostic tests can also alter this delicate balance. Fortunately, several drugs can help correct imbalances and bring the body back to homeostasis (the stability of body fluid composition and volume).
EBSCO Publishing : eBook Collection (EBSCOhost) - printed on 5/10/2020 2:40 PM via MOBERLY AREA COMM COLL AN: 2018667 ; Wilkins, Lippincott Williams &.; Pharmacology Made Incredibly Easy!
838
Electrolyte replacement drugs An electrolyte is a compound or element that carries an electric charge when dissolved in water. Electrolyte replacement drugs are inorganic or organic salts that increase depleted or deficient electrolyte levels, helping to maintain homeostasis. These drugs include: • potassium, the primary intracellular fluid (ICF) electrolyte • calcium, a major extracellular fluid (ECF) electrolyte • magnesium, an electrolyte essential for homeostasis found in ICF • sodium, the principal electrolyte in ECF necessary for homeostasis.
Potassium Potassium is the major positively charged ion (cation) in ICF. Because the body can’t store potassium, adequate amounts must be ingested daily. If this isn’t possible, potassium can be replaced orally or IV with potassium salts, such as: • potassium acetate • potassium chloride • potassium gluconate • potassium phosphate.
Pharmacokinetics (how drugs circulate) Oral potassium is absorbed readily from the GI tract. After absorption into the ECF, almost all potassium passes into the ICF. There, the enzyme adenosine triphosphatase maintains the concentration of potassium by pumping sodium out of the cell in exchange for potassium. Normal serum levels of potassium are maintained by the kidneys, which excrete most excess potassium intake. The rest is excreted in feces and sweat.
Pharmacodynamics (how drugs act) Potassium moves quickly into ICF to restore depleted potassium levels and reestablish balance. It’s an essential element in determining cell membrane potential and excitability.
Nervous about potassium? Potassium is necessary for proper functioning of all nerve and muscle cells and for nerve impulse transmission. It’s also essential for tissue growth and repair and for maintenance of acid-base balance.
Pharmacotherapeutics (how drugs are used) Potassium replacement therapy corrects hypokalemia (low levels of potassium in the blood). Hypokalemia is a common occurrence in conditions that increase potassium excretion or depletion, such as: • vomiting, diarrhea, or nasogastric suction • excessive urination • some kidney diseases • cystic fibrosis • burns • excessive antidiuretic hormone levels • therapy with a potassium-depleting diuretic 839
• • • •
laxative abuse alkalosis insufficient potassium intake from starvation, anorexia nervosa, alcoholism, or clay ingestion administration of a glucocorticoid, IV amphotericin B, vitamin B12 , folic acid, granulocyte-macrophage colony–stimulating factor, or IV solutions that contain insufficient potassium.
Be still my heart Potassium decreases the toxic effects of digoxin. Because potassium inhibits the excitability of the heart, normal potassium levels moderate the action of digoxin, reducing the chance of toxicity.
Drug interactions Potassium should be used cautiously in patients receiving potassium-sparing diuretics (such as amiloride, spironolactone, and triamterene) or angiotensin-converting enzyme (ACE) inhibitors (such as captopril, enalapril, and lisinopril) to avoid hyperkalemia.
Adverse reactions Most adverse reactions to potassium are related to the method of administration. Oral potassium sometimes causes nausea, vomiting, abdominal pain, and diarrhea. Enteric coated tablets may cause small bowel ulcerations, stenosis, hemorrhage, and obstruction. An IV infusion can cause pain at the injection site and phlebitis (vein inflammation) and, if given rapidly, cardiac arrest. Infusion of potassium in patients with decreased urine production also increases the risk of hyperkalemia.
Nursing process These nursing process steps are appropriate for patients undergoing treatment with potassium.
Assessment • Monitor the patient’s potassium level. Be particularly alert for hyperkalemia if the patient’s urine output decreases during therapy. • Monitor the patient for signs and symptoms of hyperkalemia. (See Signs and symptoms of 840
hyperkalemia, page 706.) • Watch for adverse reactions and drug interactions. • Monitor the patient’s electrocardiogram (ECG) for changes that suggest hyperkalemia, such as prolonged PR intervals; widened QRS complexes; depressed ST segments; and tall, tented T waves. • Monitor the patient’s intake and output if nausea, vomiting, or diarrhea occurs.
Before you give that drug! Signs and symptoms of hyperkalemia Potassium replacement therapy can lead to overcorrection and hyperkalemia. To prevent this, closely monitor the patient for signs and symptoms of hyperkalemia, including: • abdominal cramping • confusion • diarrhea • electrocardiogram changes (tall, tented T wave) • hypotension • irregular pulse rate • irritability • muscle weakness • nausea • paresthesia.
Key nursing diagnoses • Risk for deficient fluid volume related to adverse reactions to potassium • Decreased cardiac output related to adverse reactions to potassium • Deficient knowledge related to drug therapy
Planning outcome goals • The patient’s fluid intake and output will remain at an appropriate level for age and condition. • The patient won’t have arrhythmias. • The patient will demonstrate correct drug administration.
Implementation • Use potassium cautiously if the patient is also receiving a potassium-sparing diuretic or an ACE inhibitor. • When administering potassium IV, dilute the preparation before infusion. • Give diluted IV potassium slowly to prevent life-threatening hyperkalemia. • Never give potassium as an IV bolus or IM injection.
Nix that mix • Don’t mix IV potassium phosphate in a solution that contains calcium or magnesium because precipitates will form. 841
• Monitor the patient’s IV site regularly for signs of phlebitis. If phlebitis or pain occurs, change the site. • Give oral potassium with or after meals to minimize GI distress. • Give antiemetics or antidiarrheals as needed if the patient develops vomiting or diarrhea. • Teach the patient and caregivers about potassium therapy. (See Teaching about potassium therapy .)
Education edge Teaching about potassium therapy If potassium is prescribed, review these points with the patient and family or caregivers: • Take oral potassium with or after meals to minimize GI distress. • Dissolve all powders and tablets in at least 4 oz (120 mL) of water or fruit juice, and sip the solution slowly over 5 to 10 minutes. Also, take capsules or tablets with plenty of liquid. • Make sure not to crush or chew extended-release tablets, which will defeat the purpose of the special coating. Also understand that although the remnants of the wax matrix may appear in your stools, the drug has been absorbed. • Make sure you keep appointments for periodic blood tests to measure potassium level. • If you experience GI distress or signs and symptoms of hyperkalemia, such as diarrhea, muscle weakness, or confusion, notify your primary care provider.
Evaluation • Patient maintains adequate hydration. 842
• Patient maintains normal cardiac output as evidenced by normal vital signs and ECG. • Patient and caregivers demonstrate an understanding of drug therapy.
Calcium Calcium is a major cation in ECF. Almost all of the calcium in the body (99%) is stored in bone, where it can be mobilized if necessary. When dietary intake isn’t enough to meet metabolic needs, calcium stores in bone are reduced.
Bound, complexed, ionized Extracellular calcium exists in three forms—bound to plasma protein (mainly albumin); complexed with substances such as phosphate, citrate, or sulfate; and ionized. About 47% of the ionized calcium is physiologically active and plays a role in cellular functions.
Salting the body Chronic insufficient calcium intake can result in bone demineralization. Calcium is replaced orally or IV with calcium salts, such as: • calcium carbonate • calcium chloride • calcium citrate • calcium glubionate • calcium gluceptate • calcium gluconate • calcium lactate.
Pharmacokinetics Oral calcium is absorbed readily from the duodenum and proximal jejunum. A pH of 5 to 7, parathyroid hormone (PTH), and vitamin D all aid calcium absorption.
A soapy situation Absorption also depends on dietary factors, such as calcium binding to fiber, phytates, and oxalates, and on fatty acids, with which calcium salts form insoluble soaps. Calcium is distributed primarily in bone. Calcium salts are eliminated primarily in feces, with the remainder excreted in urine.
Pharmacodynamics Calcium moves quickly into ECF to restore calcium levels and reestablish balance. It has several vital functions: • Extracellular ionized calcium plays an essential role in normal nerve and muscle excitability. • Calcium is integral to normal functioning of the heart, kidneys, and lungs, and it affects the blood coagulation rate as well as cell membrane and capillary permeability. • Calcium is a factor in neurotransmitter and hormone activity, amino acid metabolism, vitamin B12 absorption, and gastrin secretion. • Calcium plays a major role in normal bone and tooth formation. (See Calcium in balance , page 709.)
843
Pharm function Calcium in balance Extracellular calcium levels are normally kept constant by several interrelated processes that move calcium ions into and out of ECF. Calcium enters the extracellular space through resorption of calcium ions from bone, through the absorption of dietary calcium in the GI tract, and through reabsorption of calcium from the kidneys. Calcium leaves ECF as it’s excreted in feces and urine and deposited in bone tissues. This illustration shows how calcium moves throughout the body.
Pharmacotherapeutics Calcium is helpful in treating magnesium intoxication. It also helps strengthen myocardial tissue after defibrillation or a poor response to epinephrine during resuscitation. Pregnancy and breast-feeding increase calcium requirements, as do periods of bone growth during childhood and adolescence.
844
In the IV league The major clinical indication for IV calcium is acute hypocalcemia (low serum calcium levels), which necessitates a rapid increase in serum calcium levels. Acute hypocalcemia can occur in tetany, cardiac arrest, vitamin D deficiency, parathyroid surgery, and alkalosis. IV calcium is also used to prevent a hypocalcemic reaction during exchange transfusions.
Mouth medicine Oral calcium is commonly used to supplement a calcium-deficient diet and prevent osteoporosis. Chronic hypocalcemia from such conditions as chronic hypoparathyroidism (a deficiency of PTH), osteomalacia (softening of bones), long-term glucocorticoid therapy, and plicamycin and vitamin D deficiency is also treated with oral calcium.
Drug interactions Calcium has a few significant interactions with other drugs: • Preparations administered with digoxin may cause cardiac arrhythmias. • Calcium replacement drugs may reduce the response to calcium channel blockers. • Calcium replacements may inactivate tetracyclines. • Calcium supplements may decrease the amount of atenolol available to the tissues, resulting in decreased effectiveness of the drug.
An insoluble problem • When given in total parenteral nutrition, calcium may react with phosphorus present in the solution to form insoluble calcium phosphate granules, which may find their way into pulmonary arterioles, causing emboli and possibly death.
845
Adverse reactions Calcium preparations may produce hypercalcemia if calcium levels aren’t monitored closely. Early signs include drowsiness, lethargy, muscle weakness, headache, constipation, and a metallic taste in the mouth. ECG changes that occur with elevated serum calcium levels include a shortened QT interval and heart block. Severe hypercalcemia can cause cardiac arrhythmias, cardiac arrest, and coma.
A burning issue With IV administration, calcium may cause venous irritation. IM injection of calcium may cause severe local reactions, such as burning, necrosis, and tissue sloughing.
Nursing process These nursing process steps are appropriate for patients undergoing treatment with calcium.
Assessment • Monitor the patient’s calcium level. • Monitor the patient for signs of hypercalcemia. • Watch the patient’s ECG for changes that suggest hypercalcemia.
Key nursing diagnoses • Decreased cardiac output related to calcium imbalance • Risk for injury related to osteoporosis • Deficient knowledge related to drug therapy
Planning outcome goals • The patient won’t have arrhythmias. • The patient won’t develop an increased risk of fractures. • The patient will demonstrate correct drug administration.
Implementation • Give an IV infusion slowly to prevent a high calcium level from reaching the heart and possibly causing arrhythmias and cardiac arrest. • Keep the patient recumbent for 15 minutes after injecting calcium. 846
• If extravasation occurs, stop the IV infusion and apply warm, moist compresses to the area. • Only give calcium IM in an emergency and when the IV route is impossible to use. If using the IM route, give the injection in the gluteal muscle for an adult or in the lateral thigh for an infant or young child. • Give oral calcium supplements 1 to 2 hours after meals. • Give calcium and digoxin slowly and in small amounts to avoid precipitating arrhythmias during therapy with both drugs. • Teach the patient about calcium. (See Teaching about oral calcium .)
Education edge Teaching about oral calcium If a calcium preparation is prescribed, review these points with the patient and family or caregivers: • Don’t take calcium with foods that interfere with calcium absorption, such as spinach, rhubarb, bran, whole grain cereals and breads, and fresh fruits and vegetables; take calcium tablets 1 to 2 hours after eating. • Eat foods containing vitamin D to enhance calcium absorption. • Don’t skip follow-up blood tests to monitor calcium levels. • Report signs and symptoms of hypercalcemia, including nausea and vomiting, constipation, muscle weakness, lethargy, and fatigue, to your primary care provider.
Evaluation • Patient maintains normal cardiac output as evidenced by normal vital signs and ECG. • Patient’s bone density tests remain stable over time. • Patient and caregivers demonstrate an understanding of drug therapy.
Magnesium Magnesium is the most abundant cation in ICF after potassium. It’s essential in transmitting nerve impulses to muscle and activating enzymes necessary for carbohydrate and protein metabolism. About 65% of all magnesium is in bone and 20% is in muscle.
Officiating in the ICF Magnesium stimulates PTH secretion, thus regulating ICF calcium levels.
Traffic control Magnesium also aids in cell metabolism and the movement of sodium and potassium across cell membranes.
A run on magnesium Magnesium stores may be depleted by: • malabsorption • chronic diarrhea 847
• • • • • • • •
prolonged treatment with diuretics nasogastric suctioning prolonged therapy with parenteral fluids not containing magnesium hyperaldosteronism hypoparathyroidism or hyperparathyroidism excessive release of adrenocortical hormones acute and chronic alcohol consumption drugs, such as cisplatin, aminoglycosides, cyclosporine, and amphotericin B.
Restocking the mineral stores Magnesium is typically replaced in the form of magnesium sulfate when administered IV or in the form of magnesium oxide if given orally.
Pharmacokinetics Magnesium sulfate is distributed widely throughout the body. IV magnesium sulfate acts immediately, whereas it acts within 30 minutes after IM administration. However, IM injections can be painful, induce sclerosis, and need to be repeated frequently. Magnesium sulfate isn’t metabolized and is excreted unchanged in urine; some appears in breast milk.
Pharmacodynamics Magnesium sulfate replenishes and prevents magnesium deficiencies. It also prevents or controls seizures by blocking neuromuscular transmission.
Pharmacotherapeutics IV magnesium sulfate is the drug of choice for replacement therapy in symptomatic magnesium deficiency (hypomagnesemia). It’s widely used to treat or prevent preeclamptic and eclamptic seizure activity. It’s also used to treat ventricular arrhythmias such as torsades de pointes, seizures, severe toxemia, and acute nephritis in children.
Drug interactions Magnesium has few significant interactions with other drugs: • Magnesium used with digoxin may lead to heart block.
So depressing . . . • Combining magnesium sulfate with alcohol, opioids, antianxiety drugs, barbiturates, antidepressants, hypnotics, antipsychotic drugs, or general anesthetics may increase central nervous system depressant effects. • Using magnesium sulfate with succinylcholine or tubocurarine potentiates and prolongs the neuromuscular blocking action of these drugs.
Adverse reactions Adverse reactions to magnesium sulfate can be life-threatening. They include hypotension, circulatory collapse, flushing, depressed reflexes, and respiratory paralysis. IM injections of magnesium can cause pain and induce sclerosis and must be repeated frequently.
848
Nursing process These nursing process steps are appropriate for patients undergoing treatment with magnesium.
Assessment • Monitor the patient’s intake and output. Magnesium generally isn’t given if the patient’s urine output is less than 100 mL in 4 hours. • Monitor the patient’s vital signs and ECG tracings, looking for signs of hypotension, arrhythmias, and respiratory distress. • Watch the patient’s serum electrolyte levels.
Key nursing diagnoses • Risk for deficient fluid volume related to magnesium replacement • Decreased cardiac output related to magnesium imbalance • Deficient knowledge related to drug therapy
Planning outcome goals • The patient will maintain appropriate levels of fluid intake and output for age and condition. • The patient won’t have arrhythmias. • The patient will demonstrate an understanding of drug therapy.
Implementation • Keep IV calcium gluconate available to reverse the respiratory depression that an infusion of magnesium sulfate can cause.
A knee-jerk reaction • It is of critical importance to test the patient’s knee-jerk and patellar reflexes before giving each dose. If a reflex is absent, notify the primary care provider right away and withhold the dose until the patient’s reflexes return. Otherwise, the patient may develop temporary respiratory failure and need cardiopulmonary resuscitation or IV administration of calcium. 849
• Use parenteral magnesium cautiously in a patient with renal impairment because renal impair...
Similar Free PDFs

Ele Cute - Ele cute
- 1 Pages
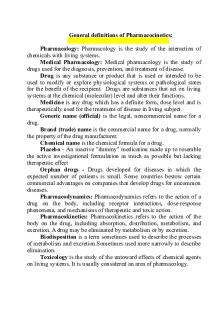
Main terms for pharmacology
- 9 Pages

Pharmacology Notes for midterm
- 95 Pages

UWorld for Nclex Pharmacology
- 16 Pages

Fluid and Electrolyte ATI
- 5 Pages

Fluid and Electrolytes
- 23 Pages

Fluid Mechanics and Hydraulics
- 5 Pages

FLUID MECHANICS AND HYDRAULICS
- 159 Pages

Fluid and Electrolytes ( Hurst)
- 4 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu






