Final Exam - Review notes PDF
| Title | Final Exam - Review notes |
|---|---|
| Course | Human Physiology and Anatomy |
| Institution | University of Connecticut |
| Pages | 92 |
| File Size | 1.9 MB |
| File Type | |
| Total Downloads | 105 |
| Total Views | 209 |
Summary
Review notes...
Description
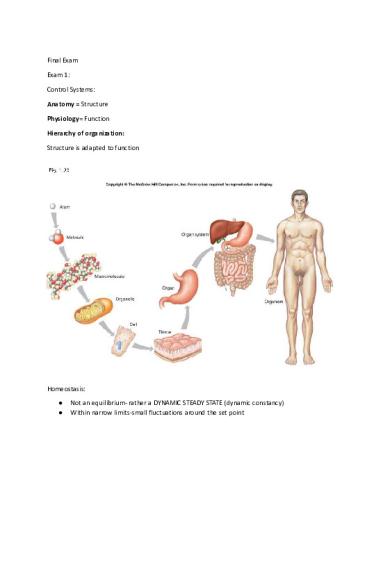
Final Exam Exam 1: Control Systems: Anatomy = Structure Physiology= Function Hierarchy of organization: Structure is adapted to function
Homeostasis: ● ●
Not an equilibrium- rather a DYNAMIC STEADY STATE (dynamic constancy) Within narrow limits-small fluctuations around the set point
Body Fluid compartments: ● ●
Intracellular fluid (67%) Extracellular fluid: o Interstitial fluid (26%) o Blood plasma (7%)
Homeostasis= dynamic steady state of conditions in the body-especially ECF Feedback control mechanisms: Components of a control system: ● ● ● ● ●
Physiological VARIABLE Set point/ Normal range (set by controller) Sensor/ Receptor (monitors variable) Integrating control center o Compares to set point and programs response Effector (carries out response)
Example of closed loop, negative feedback: This reflex response to change in body temperature functions as a negative feedback control system ●
Response returns regulated variable toward set point (response removes stimulus)
Control System of Thermoregulation
Cell Communication: To coordinate reflexes and local homeostatic responses, cells must be able to communicate with one another.
Closed loop, positive feedback
Another example is blood clotting; the tear in the vessel causes bleeding → damaged cells release chemicals → clotting begins → additional chemicals released →clotting accelerates → blood clot In summary: ● ●
Closed loop, negative feedback control keeps conditions relatively stable Closed loop, positive feedback control may promote useful change (labor contractions; blood clotting) or may causes disaster (end-stage circulatory shock)
Open Loop/ feed forward Regulation ●
Stimulus → Response – no feedback
Properties of Water Hydrogen attached to oxygen via polar covalent bonds- which give water its unique properties ● Water molecules are sticky o Hydrogen bonds are attractive force between the hydrogen attached to an electronegative atom of one molecule and an electronegative atom of a different molecule Most effective solvent Many compounds ionize → electrolytes ●
● ●
● ●
● ●
Reactivity High Heat capacity o Thermal inertia o Larger heat of vaporization Lubrication ;) Cushioning
Histology Histology = Study of Tissues
•
Tissues: Definition: Collections of cells and cell products that perform specific functions
•
Cells are organized into four main tissue types. 1. Epithelium 2. Connective 3. Nervous 4. Muscle
Every organ and structure in the body is made up of some combination of these.
Epithelial Tissue: Epithelial tissue covers or lines surfaces and cavities of the body, as well as forming secretory glands.
•
Covers exposed surfaces
•
Lines internal passageways
•
Forms glands
Characteristics of Epithelial Tissue
•
Cellularity (cell junctions) – cells connected to other cells w/o extracellular material. Cells have a regular shape.
•
Polarity (apical and basal surfaces) – characterized by presence of a free (apical) surface (that faces the outside or cavity) and an attached basal surface
•
Attachment (basal lamina/basement membrane) – anchors epithelial sheet to deeper connective tissue; produced by the epithelial cells.
•
Avascularity – “without blood vessels”
•
Regenerative – high ability to regenerate cells
Functions of Epithelial Tissue
•
Provide physical protection
•
Barrier
•
Exchange – refers to transport
•
Secretion – (glandular) – substances produced by epithelial cells released outside of cell
•
Absorption – substances brought into or across cells into body (e.g., intestinal absorption.)
➢ Basement Membrane attaches epithelia to underlying connective tissue
➢ Intercellular junctions bind epithelial cells together
➢ Desmosomes – “rivets” which mechanically connect cells to one another ➢ Hemidesmosomes – mechanical junctions which attach cells to basement membrane ➢ Tight Junctions – mechanical junctions which are impermeable – prevent substances from crossing membrane or between celsl ➢ Gap Junctions – communicating junctions which allow ions to cross (and allow for cell-cell communication.)
Classes of Epithelia
•
Based on shape and layers (Fig. 4.2M; 3.6,3.7C)
➢ Classification by SHAPE: Squamous (flat); Cuboidal; Columnar ➢ Classification by LAYERS: Simple (one layer) vs. Striated (multiple layers)
Connective Tissue
• Unlike other tissues, most connective tissues are characterized by cells and non-living extracellular (outside the cell) material called extracellular matrix •
General functions: binding, support, protection, insulation
•
Major categories: (in detail on Exam I*)
–
Connective Tissue Proper*
–
Cartilage*
–
Bone*
–
Dentin
–
Blood
–
Mesenchyme – embryonic connective tissue
General Structure of Connective Tissues
•
Specialized cells are categorized according to the connective tissue type. These cells secrete the matrix associated with the connective tissue (“blast” cells) and mature (“cyte”) cells maintain the connective tissue.
–
Fibroblasts; fibrocytes (CT proper)
–
Chondroblasts; chondrocytes (cartilage)
–
Osteoblasts; osteocytes; osteoclasts (bone)
–
Hemocytoblasts (blood)
(Suffix “blast” – refers to cells actively secreting connective tissue matrix)
–
Matrix determines function of and varies by category of connective tissue, from very loose and pliable (areolar connective tissue) to dense and hardened (bone and dentin). Matrix consists of protein fibers embedded in polysaccharide ground substance
•
There are three types of fibers:
–
Collagenous
–
Elastic
–
Reticular
Fibers: Collagenous
•
Protein collagen
– Many different types of collagen! Bone collagen differs from soft tissue collagen, for example.
•
All collagen features a stable, cross-linked triple helix
•
High tensile strength – ability to resist stretch (due to the molecular structure.)
➢ Defects in collagen cause pathophysiology of SCURVY and Osteogenesis Imperfecta
Scurvy
•
Lack of vitamin C → defective collagen synthesis –Hydroxyproline – an amino acid found rarely in other proteins, is found in collagen where it stabilizes the collagen triple helix structure
•
Symptoms due to fragile collagen: –Purpura (purple-colored spots) due to leakage of blood from small vessels under skin –Pinpoint bleeding around hair follicles, along gums, under nails –Osteoid (protein matrix of bone) formation is defective –Weakness, fatigue, aching limbs
Recall functions of connective tissue – support, protection; - these are disrupted in scurvy.
Elastic Fibers • Protein elastin, which has an unusual molecular structure in that rather than assuming a stable tertiary structure (conformation), elastin oscillates among a variety of partially-extending random coil conformations. •
Property of extensibility - can STRETCH and it will RECOIL.
Reticular Fibers
•
Protein reticulin
–
Made from Type III Collagen; looks like “immature” collagen
–
“Rete” = “net”
•
Delicate network supports individual cells in certain organs, e.g. spleen, liver
Ground Substance Made up of:
•
Interstitial fluid (part of the extracellular fluid compartment)
•
Adhesion proteins which “glue” connective tissue cells to matrix
–
Fibronectin, anchorin, laminin
•
Proteoglycans – protein cores plus long, negatively-charged polysaccharides called glycosaminoglycans (“GAGs”). Depending upon the type of GAGs found in the matrix, the ECF may be converted from a fluid to a semi-solid gel.
Categories of Connective Tissue Proper:
Loose Connective Tissue 1) Areolar connective tissue – “filler”; loose meshwork w/ all three fiber types; also contains cells (mast cells, macrophages, lymphocytes) important in body’s defense. 2) Adipose (fat) tissue: adipose tissue fat stored in fat vacuoles associated w/ each adipocyte. 3) Reticular connective tissue – framework supporting glands
Dense Connective Tissue a) Dense Regular – makes up ligaments and tendons. Lots of collagen (tensile strength) arranged in parallel bands. Resists stretch primarily in one direction (e.g., line of pull for muscle’s tendinous insertion.) b) Dense Irregular – makes up dermis of skin; also lots of collagen for tensile strength, but irregularly arranged. Thus skin can resist stretch in all directions. c) Elastic Connective Tissue
Cartilage – General Structure
•
Cells
–
Chondroblasts
–
• Produce matrix; once surround themselves w/ matrix they mature into… Chondrocytes
•
• Mature cartilage cells, function to regulate and maintain cartilage. If they die, cartilage disintegrates. • Located in lacunae (“islands”) Matrix
–
Protein fibers – type and proportion varies w/ cartilage type
–
Ground substance
• GAGs include chondroitin sulfates, which convert interstitial fluid into a …. • firm gel • A connective tissue perichondrium (“around cartilage”) surrounds most cartilage structures.
•
Cartilage is avascular
Hyaline Cartilage
•
Matrix: lots of dense, fine collagen.
•
Perichondrium
–
dense CT membrane
–
Surrounds hyaline cartilage
•
Strong, flexible and SMOOTH
•
Articular cartilage of joints = one example
•
Function: Reduces friction in joints
Fibrocartilage
•
Matrix: Collagen, some elastic fibers
•
Example: Intervertebral disks
•
Function: Resists compression
– How? Even soft tissues like fibrocartilage can be effective at resisting compressive forces due to the water in the matrix
Bone Tissue
•
Bone matrix has 2 components
–
ORGANIC (protein; primarily collagen; called “osteoid”)
–
INORGANIC (mineral; primarily Calcium Phosphate)
Histology of Bone: Cells
•
Osteoblasts
– Bone Building – secrete organic matrix (“osteoid” – protein matrix consisting largely of bone collagen.) As they surround themselves w/ osteoid, they mature into…
•
Osteocytes
– Mature bone cells – maintain bone matrix; role in metabolism; if osteocytes die, bone erodes.
A third type of “bone cell” actually derives from a type of white blood cell:
•
Osteoclasts
– Break down bone. Osteoclasts contain proteolytic enzymes to break down bone protein, and acid hydrolase enzymes to dissolve mineral matrix. They are a normal feature of bone tissue – normal bone metabolism / turnover requires both bone building and bone breakdown cells.
Histology of Bone: Matrix
•
Organic (Protein) = Osteoid
–
1/3 bone mass
–
Collagen
– Property: Bone collagen (like all collagen) confers the property of tensile strength – resists stretch. Organic matrix is necessary for “tough” bones. Without it – bones would be too brittle to resist the pull of tendons when muscles contract.
•
Mineral (inorganic) Matrix
•
2/3 of bone matrix is calcium phosphate, Ca3(PO4)2:
– reacts with calcium hydroxide, Ca(OH)2 to form long (up to several millimeters!), needle-shaped crystals of Hydroxyapatite: Ca10(PO4)6(OH)2 which are secreted onto the protein matrix of bone during the ossification process.
•
Property: The inorganic matrix allows bone to resist compressive forces.
SKIN – Integumentary System Structure of Skin
•
EPIDERMIS = Epithelial Tissue: stratified squamous keratinizing epithelium to form a waterproof covering Other cells include melanocytes (pigment melanin) and various immune and sensory cells.
•
DERMIS = Connective Tissue
SUBCUTANEOUS TISSUE (Hypodermis) Not technically part of “skin”
Epidermis Structure
•
Stratified Squamous Keratinizing Epithelium
•
Avascular: Like all epithelial structures, the epidermis has no blood vessels.
•
Five layers in thick skin
–
Outermost layer = dead, keratinized cells
•
Layers of Epidermis
–
Stratum Corneum: Outermost/most superficial layer; dead flat keratin-filled cells.
–
Stratum Lucidum: Dead cells, anucleate (no organelles at all); seen in thick skin
– Stratum Granulosum: Granules (of keratin) visible in this layer; process of kertinization begins here. Protein keratin forms filaments, fills the cell
Stratum Spinosum: almost all are amitotic (cannot divide;) are living cells connected by desmosomes.
–
–
Stratum Basale: Regenerative layer; cells divide continuously.
Dermis Structure The dermis contains blood vessels, free nerve endings, oil and sweat glands (which derive from epidermis but are located in dermis. Two Connective Tissue Layers:
•
Outer Papillary layer
– Areolar C.T.; forms dermal papillae (projections) to connect with overlying epidermis and supply blood via capillaries. Contains defense cells such as macrophages and mast cells in addition to fibroblasts (CT cells.) –
Blood vessels, lymphatic vessels, nerve endings, sweat glands found here.
•
Inner Reticular layer
–
Dense Irregular C.T. – resists stretch in all directions.
Hypodermis
•
AKA Subcutaneous Layer; Superficial Fascia
•
Areolar connective tissue
•
In addition to fibroblasts; – Macrophages: ingest bacteria, etc.; phagocytosis – Mast cells: secrete histamine (inflammatory mediator)
•
Role in body’s defense – “first line” to prevent bacteria and other pathogens from entering bloodstream.
Functions of Skin
•
Protection: chemical, physical and biological barriers
•
Temperature regulation: controlling amount of heat lost from body via peripheral vasodilation (opening of blood vessels) or vasoconstricton (closing.)
•
Sensation: many types of sensory receptors found in skin, including temperature, pressure, touch, vibration, pain…giving information about conditions in the external environment.
•
Metabolic / vitamin D, e.g.: activation of Vitamin D by action of ultraviolet light
•
Some excretion (small amounts of nitrogenous wastes)
•
Blood reservoir
Bone Physiology Notes
Functions of Bone / Skeleton
•
Support: Framework for the body
•
Protection: especially of vital organs (heart, lung) and brain
•
Allow movement / lever system: due to structure of joints (articulations)
•
Storage depot for Ca and P salts – homeostasis of these electrolytes (especially Ca++) is
vital
•
Hemopoiesis: “blood forming” – all blood cells develop in bone marrow
Classes of Bone
•
Long Bones
•
Short Bones
•
Flat Bones
•
Irregular Bones
•
Sesamoid Bones
Gross Structure – Long Bone •
Diaphysis: Shaft of long bone; composed of compact bone; hollow inside.
•
Metaphysis: between diaphysis and epiphysis (‘end’)
• Epiphysis: End of long bone – proximal (closest to midline) epiphysis and distal (furthest from midline) epiphysis. Thus for humerus – proximal epiphysis is close to shoulder joint; distal is close to elbow joint. • Epiphyseal disk: Consists of hyaline cartilage; site of growth (in length) of a long bone, AKA (also known as) growth plate or epiphyseal plate. • Epiphyseal line: “Closure” (ossification of) epiphyses once growth is complete leaves a line which is a remnant of that growth plate. • Marrow Cavity – AKA medullary cavity – hollow diaphysis of long bone; filled with bone marrow. Red (active) – Erythropoiesis (blood formation) occurs here; found in marrow cavity of young children / infants; also found in other spaces within bone (including proximal epiphyses of humerus and femur in adults.) –
Yellow (inactive) – lots of fat, found in adult marrow cavities; capable of converting to active red marrow.
–
• Spongy Bone – Found in epiphyses / metaphyses of long bones; AKA spongy bone; histology follows. • Compact Bone – found in diaphyses of long bones; outer layers of bones; histology follows. •
Articular Cartilage – hyaline cartilage covering articular surfaces of bones
• Periosteum – Dense connective tissue membrane surrounding bone – source of osteogenic cells → osteoblasts. • Endosteum – Dense connective tissue membrane lining marrow cavity; source of osteogenic cells.
Blood Supply
•
Bone is a dynamic tissue; constantly undergoing remodeling and turnover (breakdown/build up to keep strong) – Responds to mechanical stress; for example, weight training increases bone density. Conversely, inactivity leads to bone breakdown.
•
Unlike cartilage, bone is very vascularized. If blood supply is damanged, bone will die.
–
Blood vessels enter compact bone via Volkmann’s canals
Components of Bone
Compact Bone Tissue has a very organized structure. It is dense, very strong, but heavy.
•
Unit of compact bone = Haversian System (Osteon) which is seen in cross-section.
–
Haversian (central) canal - contains blood supply for osteon
–
Lamellae – rings of mineralized bone matrix surrounding Haversian canal.
–
Lacunae (“holes”) contain osteocytes – mature bone cells.
– Canaliculi – “tunnels”, containing ECF (extracellular fluid) which connect adjacent lamellae, and supply osteocytes with nutrients (which enter ECF from blood vessels in Haversian canals)
Similar Free PDFs

Final Exam - Review notes
- 92 Pages

Final Exam Review Notes
- 18 Pages

Final Exam Review Notes
- 17 Pages

Chem Final Exam Review
- 12 Pages

Bio Final Exam Review
- 2 Pages
Final EXAM Review booklet
- 5 Pages

CHEM303 final exam review
- 4 Pages

Psychology Final Exam - Review
- 13 Pages

Jarvis Final Exam Review
- 12 Pages

Final exam review
- 96 Pages

Final Exam Review
- 48 Pages

Marketing Final Exam Review
- 15 Pages

Final exam review
- 8 Pages

Astronomy Final Exam Review
- 2 Pages

Final Exam Review Guide
- 4 Pages

Final exam review flsp4420
- 5 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu