Final Exam Review PDF

| Title | Final Exam Review |
|---|---|
| Author | Sarah Peebles |
| Course | Nursing Professionalism and Ethics |
| Institution | Algonquin College |
| Pages | 31 |
| File Size | 581.4 KB |
| File Type | |
| Total Downloads | 100 |
| Total Views | 135 |
Summary
Exam review...
Description
NURSING ETHICS FINAL EXAM REVIEW 5 components of nurse-client relationship o trust, respect, professional intimacy, empathy and power Informed consent requires (5 things): o Competence, Amount and accuracy of information, Patient understanding, Voluntariness, and Authorization 4 strategies that a nurse can implement to prevent unresolved conflict from hindering client care: a) promote a respectful work environment by modelling professional behaviours;23 b) mentor, support and integrate new staff members into the practice setting;24 c) reflect on personal attitudes, motivators, values and beliefs that affect relationships with colleagues, identify personal areas in need of improvement and strive to alter their own behaviour in situations that have previously ended in conflict; and d) recognize that personal stress may affect professional relationships and take steps to manage that stress. Culturally sensitivity care: communication, interpreters, non verbal strategies, what patients view of hospital, nurses, religious customs and rituals Identify 7 CNO professional standards revised 2002: o Accountability o Continuing Competence o Ethics o Knowledge o Knowledge Application o Leadership o Relationships 3 RN practice to client care: the nurse, client and the environment Legislation for refusing work when health safety of the worker is in danger: Right to Refuse by OHSA CNO can investigate allegations; they can’t terminate employment of nurses 7 categories of necessary entry-to-practice capabilities that can be used to gauge personal fit to be a profession: requisite skills and abilities o Protection of the Public o Practice References o Approval of Nursing Education Programs
o o o o
Registration and Membership Requirements Legal Reference Public Information Continuing Competence
Permits the sharing of personal health information… PHIPPA Legislative requirement for all nurses working in the province of Ontario canada Self reflection RHPA scope of practice established controlled acts ABOUT THE CNO
Responsible in regulation ~160,000 nurses in Ontario. CNO mission is to regulate nursing in the public interest. (public protection) CNO legislative frameworks are from RHPA 1991 & Nursing Act 1991. The College’s role: 1. Articulating and promoting practice standards. 2. Establishing requirements for entry to practice. 3. Administering a Quality Assurance Program. 4. Enforcing standards of practice and conduct. 5 Statutory Committees: 1. Discipline 2. Fitness to Practice 3. Inquiries, Complaints and Reports 4. Quality Assurance 5. Registration
National Competencies in the Context of Entry-Level RN Practice
Purpose of Entry-Level Competencies: o Protection of the Public o Practice References o Approval of Nursing Education Programs o Registration and Membership Requirements o Legal Reference o Public Information o Continuing Competence Published by the College in 2005 to align with the regulation change towards university baccalaureate education requirements. Revised by Jurisdictional Collaborative Project (JCP) represented by 10 provincial and territorial nursing regulatory bodies in Canada. Aim: o enhance jurisdictional consistencies in entry-level competencies for registered nurses that is based on a common competencies framework
o utilize the competencies framework to support the Mutual Recognition Agreement about reciprocity of registered nurse registration within Canada o ensure that the entry-level competencies are evidence-informed and reflect new developments in society, health care, nursing knowledge and current best practice.
Guiding Principles: (8) o Requisite skills and abilities are required to successfully attain the entrylevel registered nurse competencies. o Entry-level registered nurses have a strong foundation in nursing theory, concepts and knowledge, health and sciences, humanities, research, and ethics. o Entry-level registered nurses are prepared at the university baccalaureate education level as generalists to enter into practice safely, competently and ethically o Competencies of the entry-level registered nurse are applicable across all practice settings o Entry-level registered nurses are expected to practise in a manner consistent with provincial and federal legislation that directs nursing practice, in addition to the College’s standards for professional practice and ethics o Entry-level registered nurses are responsible for critical reflection and assessment of their practice in relation to their ability to meet the competencies, including obtaining the necessary education in order to attain and maintain competence o Entry-level registered nurses actively engage in interprofessional collaborative practice essential for improvement in client health outcomes o Entry-level registered nurses are practitioners whose level of practice, autonomy and proficiency grow through collaboration, mentoring and support from registered nurse colleagues, leadership and the interprofessional health care team
Competency: defined as the knowledge, skill, ability and judgment, required for safe and ethical nursing practice
Conceptual Framework: (5 broad competency categories) o Professional Responsibility and Accountability: Consistently demonstrates professional conduct in accordance with the College’s standards for nursing practice and ethics; and that the primary duty is to the client to ensure safe, competent, ethical nursing care. o Knowledge-Based Practice: Specialized Body of Knowledge & Competent Application of Knowledge. (1) Draws on diverse sources of knowledge and ways of knowing; including the integration of nursing knowledge from the sciences, humanities, research, ethics, spirituality, relational practice, critical inquiry and primary health care principles. (2) Demonstrates competency in the provision of nursing care. The competency statements in this section apply to the four areas of nursing care: Assessment, Planning, Implementation of Care and Evaluation. The provision of nursing care is an iterative process of critical inquiry and is not linear in nature.
(2): ongoing comprehensive assessment, collaborating with clients to develop health care plans, providing RN care, ongoing evaluation of client care
o Ethical Practice: Demonstrates competency in professional judgment and practice decisions by applying the ethical values and responsibilities in the College’s standards for ethics. The registered nurse also engages in critical inquiry to inform clinical decision-making, and establishes therapeutic, caring, and culturally safe relationships with clients and the interprofessional health care team. o Service to the Public: Demonstrates an understanding of the concept of public protection and the duty to provide and improve health care services in collaboration with clients and other members of the interprofessional health care team, stakeholders and policy makers o Self Regulation: Demonstrates an understanding of professional selfregulation by advocating in the public interest, developing and enhancing one’s own competence, and ensuring safe practice VOCAB: Accountability: An obligation to the public to accept responsibility for (explain) one’s actions and conduct, in accordance with legislative requirements and standards of the nursing profession.
Competencies: The integrated knowledge, skills, abilities and judgment required to practise nursing safely and ethically. Competent: The demonstration of integrated knowledge, skills, abilities and judgment required to practise nursing safely and ethically. Individual Competence: The nurse’s independent ability to use her/his knowledge, skill, judgment, attitudes, values and beliefs to perform in a given role, situation and practice setting Continuing Competence: The ongoing commitment of a registered nurse to integrate and apply the knowledge, skills and judgment with the attitudes, values and beliefs required to practice safely, effectively and ethically in a designated role and setting Scope of Practice: Roles, functions, and accountabilities that registered nurses are legislated, educated, and authorized to perform, as defined in Section 3 of the Nursing Act, 1991: “The practice of nursing is the promotion of health and assessment of, the provision of, care for, and the treatment of, health conditions by supportive, preventive, therapeutic, palliative and rehabilitative means in order to attain or maintain optimal function.” CONFIDENTIALITY AND PRIVACY – PERSONAL HEALTH INFORMATION
The Personal Health Information Protection Act, 2004 (PHIPA) governs health care information privacy in Ontario. PHIPA sets consistent rules for the management of personal health information and outlines the client’s rights regarding his/her personal health information. The Quality of Care Information Protection Act (QOCIPA) is another piece of legislation for the health care sector. Its purpose is to promote open discussion of adverse events, peer review activities and quality of care information, while protecting this information from being used in litigation or accessed by clients. This means that nurses’ activities and records associated with the College’s Quality Assurance Program cannot be used in legal proceedings. A custodian is an organization that provides care within the health care continuum. Nurses who are employees or volunteers, or contracted or credentialed by health care organizations (e.g., clinics, laboratories, CCACs, hospitals and longterm care facilities), are considered “agents” of a custodian. The legislation defines agents as people authorized to act for, or on behalf of, a custodian Nurses in independent practice, or those employed in health services in nonhealth care settings (e.g., OHNs), are considered custodians. The legislation also outlines permitted disclosures that do not require client consent. The legislations permitted disclosures that do not require client consent.
o Implied Consent: It is a custodian’s obligation to fulfill these conditions by posting a notice or providing a brochure that describes the purposes for the collection, use and disclosure of personal health information. This kind of notice is one way to fulfill the conditions for implied consent. o Express Consent: PHIPA does not require a specific form of express consent, which may be given verbally or in written form. It may be provided over the telephone or electronically if the nurse is sufficiently able to identify the person; however, express consent that is written helps avoid ambiguity. Express consent is required if: info is to be disclosed outside the health care team (ex. insurance company), info is used for fundraising, info is being collected for marketing research/activities. o Substitute Decision Makers: spouse or parent of a child under 16 years old. The legislation recognizes that personal health information belongs to clients and is simply being housed in health care facilities. Clients have the right to give, refuse or withdraw their consent to the collection, use and disclosure of their personal health information. Lockbox Provision: clients have the right to instruct that a part of their personal health information not be shared with other providers. The nurse must advise other hcp that some relevant information has been withheld at the direction of the client. Clients can correct their information; they can request to change it only if the record is inaccurate or incomplete. Possible grounds for refused access to PHIPA: information are generated for Quality Assurance program, a raw data, access to the information would reveal the identity of a confidential source of information. Disclosure: defined as making information available or releasing it to another custodian or person. Professional Misconduct: Nursing Act 1991 “giving information about a client to a person other than the client or his or her authorized representative, except with the consent of the client or his or her representative, or as required or allowed by law.”
Standard Statements
Personal health information practices Knowledgeable consent and substitute decision-makers Client’s right to access and amend his/her personal health info Potential for harm Disclosure without consent: ex. Child and Family Services Act 1990, Children’s Aid Society
Maintaining Quality Practice Settings
Care delivery processes: delivery of care related to confidentiality and privacy Communication systems: info sharing via electronic system should be secure Leadership: process of supporting others Professional development systems: promotes a learning environment
DECISIONS ABOUT PROCEDURES AND AUTHORITY Expectations of nurses to determine if: they have the authority to perform a procedure, is it appropriate for them to perform a particular procedure, and if they are competent to perform the procedure. -
Procedures that are authorized in Nursing Act 1991, those delegated, those carried out in emergencies, those that do not fall within the controlled act. 4 Standards (Decision Tree) 1. Appropriate Health Care Provider: if the procedure promotes safe client care and if the nurse is appropriate to perform the procedure. 2. Authority: Nurses must ensure they have the appropriate authority before performing a procedure (ex. orders, directives, delegation). 3. Competence: competent in both cognitive and technical aspects prior to performing a procedure. 4. Managing Outcomes: ensure to identify potential outcomes of the procedure, have authority and competence to manage the outcomes, and have resources available to manage those outcomes. Decisions about performing procedures: Client, Nurse and Environment
VOCAB: Authorizing mechanism. An authorizing mechanism is a means by which the authority to perform a procedure is obtained or the decision is made to perform a procedure. The appropriate authorizing mechanism depends on the nurse’s category or class, role and practice setting. Examples of authorizing mechanisms include orders, initiation, directives and delegation. Delegation. Delegation is a formal process that transfers the authority to perform a controlled act. A regulated health professional who has the legislated authority and competence to perform a procedure within one of the controlled acts can delegate that procedure to others. (Delegation may include an order) Direct client order. A client-specific order can be an order for a procedure, treatment, drug or intervention for an individual client. An individual practitioner directs a specific intervention to be performed at a specific time(s) for a specific client. A direct order may be written or oral; for example, given by telephone. Preprinted
orders are supportive tools that require a client’s name, the date and an authorizing signature before implementation. Directive. A directive is an order for a procedure, treatment, drug or intervention that may be implemented for a number of clients when specific conditions are met and specific circumstances exist. Most often a directive is a physician’s order, and it is always written. Initiation. Regulations under the Nursing Act give RNs and RPNs who meet certain conditions have the authority to initiate specific controlled acts. Order. An order is a prescription for a procedure, treatment, drug or intervention.
Professional misconduct. 1. Contravening a standard of practice of the profession or failing to meet the standard of practice of the profession. 2. Directing a member, student or other health care team member to perform nursing functions for which she or he is not adequately trained or competent to perform. 3. Failing to inform the member’s employer of her or his inability to accept specific responsibility in areas in which specific training is required or for which the member is not competent to function without supervision. 4. Contravening a provision of the Nursing Act, the Regulated Health Professions Act, 1991 or regulations under either of those acts. RHPA Regulated Health Professions Act 1991 – scope of practice of various health professions may overlap. RHPA established 13 controlled acts but only 4 are authorized to RNs. 1. Scope of practice statements 2. Controlled acts authorized to the profession Four controlled acts authorized to RNs: RNs can DO 1. Performing a prescribed procedure below the dermis or a mucous membrane. 2. Administering a substance by injection or inhalation i. ii.
beyond the external ear canal, beyond the point in the nasal passages where they normally narrow,
iii.
beyond the larynx,
iv.
beyond the opening of the urethra,
v.
beyond the labia majora,
vi.
beyond the anal verge, or
vii.
into an artificial opening into the body.
3. Putting an instrument, hand or finger 4. Dispensing a drug
Exceptions to the need of Authorization: o Emergency, first aid o Under supervision or direction of a member of the profession (ex. student with clinical instructor) o Treating a member of a person’s household o When assisting with routine activities of living
Nursing Act 1991 - scope of practice statement that describes in a general way what the profession does and the methods that it uses. For Nursing: “The practice of nursing is the promotion of health and the assessment of, the provision of, care for, and the treatment of, health conditions by supportive, preventive, therapeutic, palliative and rehabilitative means in order to attain or maintain optimal function “
DOCUMENTATION Documentation—whether paper, electronic, audio or visual — is used to monitor a client’s progress and communicate with other care providers. It also reflects the nursing care that is provided to a client. Nursing Documentation:
Reflects client’s perspective and promotes continuity of care.
Communicates to all HCP of the plan of care, interventions and outcomes.
Interprofessional documentation within the client record.
Demonstrates nurses commitment to providing safe, ethical and effective care.
Application of nursing knowledge, skill and judgment.
Standard Statements: Communication, Accountability, & Security ETHICS To make decisions about ethical situations, nurses need to be aware of their personal values. They need to be knowledgeable of clinical situations and ethics, and they require the ability to think through a problem and reach a sound decision that they can explain and justify by referring to ethical values.
7 Ethical Values: CNO has identified the following values as being most important in providing nursing care in Ontario: Client well-being – facilitating client’s health and welfare, and preventing/removing harm. Nurses must use the client’s views. Client choice – means self determination, includes the right to the information necessary to make choices and to consent or refuse care. When clients have the right information, they can decide what is best for themselves. o Limits to choice: clients do not have the right to choose/cause harm. o Values differ from nurses: If the nurse believes he/she cannot provide care, the nurse needs to arrange for another caregiver and withdraw from the situation. If there is no other caregiver, the nurse must provide the immediate care required. o Behavioral directives: respecting client’s wishes even if not the same as theirs. Privacy & Confidentiality – Nurses must provide care that maintains dignity and privacy of clients. Respect for life – Needs to be respected, protected and treated with consideration. Consideration of quality of life. Maintaining commitments – meeting obligations towards clients, themselves, the...
Similar Free PDFs

Chem Final Exam Review
- 12 Pages

Final Exam - Review notes
- 92 Pages

Bio Final Exam Review
- 2 Pages
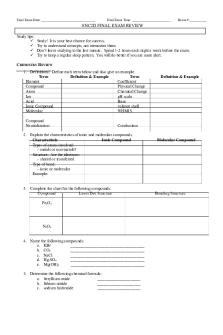
Final EXAM Review booklet
- 5 Pages

CHEM303 final exam review
- 4 Pages

Psychology Final Exam - Review
- 13 Pages

Jarvis Final Exam Review
- 12 Pages

Final exam review
- 96 Pages

Final Exam Review
- 48 Pages

Marketing Final Exam Review
- 15 Pages

Final exam review
- 8 Pages

Astronomy Final Exam Review
- 2 Pages

Final Exam Review Guide
- 4 Pages

Final exam review flsp4420
- 5 Pages

Theo Final Exam Review
- 16 Pages

Entrepreneurship final exam review
- 33 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu