3 - Musculoskeletal or Articular Dysfunction PDF

| Title | 3 - Musculoskeletal or Articular Dysfunction |
|---|---|
| Course | Nursing Care Of Childrearing Families |
| Institution | University of Nevada, Las Vegas |
| Pages | 17 |
| File Size | 740.3 KB |
| File Type | |
| Total Downloads | 74 |
| Total Views | 150 |
Summary
Notes...
Description
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION FRACTURES
•
•
Child vs Infant Assessment – 6 Ps (Pain, pulselessness, pallor, paresthesia, paralysis, pressure) Epiphyseal injuries o Located in the long that allows us to grow and allows us to grow taller. Weakest part of your bone Goal o Establish alignment Splinting it, pulling them back into place, or surgery (compound fractures since there are little pieces of bones) It is important to do this in a timely manner because kids heal faster than adults o Prevent diminish 6 P’s
Children are susceptible to factures •
Natural tendency toward active mobility
•
Limited gross motor coordination
Infants •
• •
True accidents causing fractures are rare •
Infants should not have fractures because they do not move. They’re not crawling, walking, running
•
The only one that’s pretty common in this age group is clavicle fractures. Going through that birth canal can cause some issue but if there’s any other type of long bone fractures then we want to investigate this further
Investigate further
Common in childhood •
Forearm fractures •
•
They are running around; they are not very coordinated. They tend to topple forward to fall. They put their arm out and then fracture their forearm.
clavicle
•
Sports are a common cause of injury
•
Epiphyseal Injuries •
Epiphyseal plate allows long bones to grow and for us to get taller. Weakest point – children who have these are more susceptible to having fractures. With the epiphyseal injuries, we are worried if these go diagonally through the epiphyseal plate then we’re worried that the long bones are not going to grow at the same rate as the other one that mirrors that so we want to look where is it, a horizontal and vertical. If it it’s diagonally through these epiphyseal plates then we’ll watch that area a lot more closely to make sure that it’s growing and healing at the same rate as the other ones.
• •
•
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION May cause problems if fracture line is not transverse
Muscle contracts to splint injury after fracture occurs •
May pull bone ends out of alignment
•
When a child fractures their bone, they have some protective measures that their body does to keep it in place or to try to protect that area that has broken so your muscles actually contract around that area and unfortunately when those muscles contract around that broken bone, it may actually pull the bone even more out of alignment. It’s not always necessarily the bone that is causing the problem, it could be those muscles trying to protect itself and actually making situation worse. We want to make sure that we’re doing when we have a child that comes in and we’re suspecting a fracture is assess the six Ps.
Assess the 6 P’s •
Pain
•
Pulselessness
•
Pallor
•
Paresthesia
•
Paralysis
•
Pressure
•
Determine the mechanism of injury. if the bone is sticking outside of the skin then we want to cover that wound and clean it with a sterile dressing. Only because then we have that increased risk of infection and want to try to stabilize and mobilize that limb so that we’re not moving it around and causing more and more damage. We want to elevate any type of fractures elevation, decrease swelling, and decrease any other issues that it’s having.
•
Clinical manifestations •
Generalized swelling
•
Pain/tenderness
•
Diminished function
•
Bruising
•
Muscular rigidity
•
Crepitus
•
If child will not allow you to touch them •
• •
Sometimes the child won’t allow you to touch the area in order to do your full assessment and so anything that you can have them do to help you such as wiggling their own fingers, can they pinch on the tip of their fingernail to see capillary refill. If you can have them help and assist you in getting all of that information is absolutely very helpful.
Have them point to where it hurts and wiggle fingers
Diagnosis
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION • •
X-ray
Fracture management goals •
Reestablish alignment
•
Retain alignment and length
•
Restore function
•
Prevent further injury and deformity
•
Pain management
•
Casts may be delayed
•
•
Due to swelling
•
We do not want to put cast on right away after this child has fractured and we have realigned their bone. After the realignment, we typically will put on a splint and then send them home. They’ll follow up with that orthopedic doctor a couple days later once that swelling is decreased.
•
If we cast them right away then once that swelling goes down then that arm is there, the leg or wherever, whatever that fracture is it’s just going to kind of be moving around inside the cast and that alignment won’t be maintained as well as we want it to so we don’t delay putting those casts on just because of swelling.
Children heal quickly •
Thickened periosteum
•
Generous blood supply
•
Kids heal very very quickly so it’s important to get the bone realigned as quickly as possible so that healing can occur. Kids can be back out and up and running and back everything is normal within four weeks and it’s really important to get that alignment reestablished and to keep it aligned.
Fracture Complications
Compartment Syndrome
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION The swelling within this enclosed space and then it causes that pressure which causes decreased circulation movement that occur as little as 20 minutes. it’s important to detect and we want to make sure that we’re assessing those six Ps. The biggest signs and symptoms that are related to deterioration around this neuromuscular status or compartment syndrome is going to be motor weakness (unable to move very well), pain (pain changes), palpable pulse in a capillary refill. You won’t be able to move it. Treatment for compartment syndrome was to immediately relief that pressure. If it’s on a cast then cut the cast to relieve pressure. Do not elevate. If you elevate the arm that arm is going to come out of the arm and there is no way for it to get back up because there is so much pressure in there. The deterioration is going to happen a whole lot faster so don’t elevate this the way you would to decrease any type of swelling. You want to keep the extremity or whatever is having compartments syndrome at the level of the heart. Putting something in can make you scratch, you get a break in the skin, it can cause infection leading to swelling. Swelling pushing against the cast doesn’t have anywhere to go so it is going to cause pressure. It is going to put pressure on muscles, tendons, skin circulation will have issues. Relieve pressure by cutting off the cast.
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION Child in a cast Majority of the time we will not see cast in the hospital again. The child come in and break their arm. When we align and reset, we split and send them home. The cast is done in the orthopedic office and so if you’re seeing a cast, you’re seeing this because a child has come into the hospital for some other reason and they just so happen to have a cast on we do need to make sure that we assessing it or they’re some sort of a spica cast. Spidca cast or whenever we’re casting anybody. The whole idea behind cast is to maintain that alignment and so how they determine what type of cast they put on or kind of how big that cast is to make sure that stays indelayed alignment Cast placement place. Assessment of cast •
Immobilize the joint above and below the fracture •
•
•
•
The cast will come from hand all the way up past my elbow to maintain that alignment
•
We don’t typically put a cast on a child that breaks their arm in the ER. We realign it, we splint it and we send them home. Splint it and let the swelling to go down and then they’ll cast it a few days later in the orthopedic office
Keep cast clean and dry We need to make sure we keep these cast clean and dry
Do not put anything in the cast •
•
A fracture in the forearm then you need to immobilize the joint below which is going to be the wrist and the joint above the elbow in order to keep that bone in alignment.
Cast purpose: to maintain alignment
• •
Elevation o When to elevate Hot spots – infections
Putting stuff down the cast is it’s a moist hot environment. If we break the skin now, we have this great environment for infection
Do not dry with fans •
We want that cast to heal on its own from internal to external again while looking at those 6 Ps.
•
Immediately report the 5P’s of ischemia
•
Evaluate “hot spots” on surface or foul-smelling areas of the cast •
If you take your hand and you put your bare hands on top of a cast and feel around. If there is any type of an infection underneath that cast when you get right above that infection on the cast, you’ll touch the cast and it’ll actually be hot or what we call hotspots
Sprains and Strains – we see it more in the ER situation
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION •
•
•
Sprain: •
When trauma to a joint causes a ligament to either stretch or partially or completely tear
•
Often accompanied by damage to blood vessels, muscles, tendons, and nerves
•
Joint “feels loose”, “snap”, or “pop”
•
Rapid onset of swelling
•
Immediate disability and reluctance to use joint
•
Very common in ankle sprains when you were running and then all of a sudden you feel like a snap or a pop and then they don’t want to use that joint anymore
Strain: •
A microscopic tear to the musculotendinous unit
•
Area is painful to touch and swollen
•
Usually happens over time
•
The more rapid the strain occurs the more severe
6-24 hours the most critical period •
Ice injury immediately
•
Ice the injury and immediately. Do RICE and ICE management.
•
Therapy should be intermittent
•
No longer than 30 minutes at a time •
To prevent tissue injury
•
Elevate the extremity
•
A lot of times people want to take their shoe off to see what’s going on. You actually want to put ice on it, the compression is kept that show on actually taking that shoe lace and making that shoe a lot tighter for compression while you elevate ice on it. It is going to be really important.
•
ICE should be an intermittent therapy. No longer than 30 minutes at a time and it doesn’t have to be like arctic cod. It needs to make sure that it’s reducing the swelling but you don’t want to leave it on there for five hours so 30 minutes on and 30 minutes off
Legg-Calve’-Perthes Disease
•
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION Aseptic necrosis of the femoral head •
A temporary disturbance of circulation to the femoral capital epiphysis
•
Self-limiting disorder
•
Process may take 18 months to several years
•
Reformed femoral head may appear severely altered or completely normal
•
Affects children 2-12 yrs •
Most cases boys 4-8yrs
•
Unknown cause
•
The nice round joint that goes into your hip that allows your leg to move becomes flattened out and so that round ball is in there moving around freely and so you have this decreased ROM and pain.
Clinical Manifestations •
Insidious onset – very slowly comes on
•
Intermittent limp on affected side •
Most apparent in the morning or after a long day of activities
•
Hip soreness
•
Pain
•
Joint dysfunction
•
Limited range of motion – femoral head has been flattened out
•
Diagnosis •
•
Established by X-ray and MRI
Ultimate outcome depends on: •
Early identification
•
Efficient treatment
•
Child’s age at onset
•
Younger the age better prognosis •
5yrs and younger have best outcome
•
Good compliance = excellent prognosis
•
Conservative therapy •
Bracing/casts
• •
•
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION Continued for 2-4 years The cast is right in our hip joint and so that means there is a spica cast meaning that they have the cast from their chest all the way down past their knee. They won’t be able to walk, run, play sports. It typically happens between the ages of 4 and 8. Having them in cast for 2 to 4 years is a huge detriment to their physical and mental wellbeing.
Surgical correction •
Return to normal activity in 3-4 months after intensive physical therapy so most families do opt to have more invasive surgical correction. Most families opt to have the surgical correction.
•
Education
•
Growth and development activities
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION Scoliosis •
Complex spinal deformity in 3 planes
•
Usually: lateral deviation or curvature of the spine •
•
Types •
•
•
•
•
Usually >10 Degrees
Congenital •
Occurs in fetal development
•
Look at 18 weeks ultrasound – spine, the heart, and all of the organs
Infantile •
Birth to age 3
•
We are going to discover this when they are coming in for their well child visits. We’re going to be looking at their spine, pulling their legs out to make sure that those legs are coming in evenly and looking at all of their chunky monkey folds to make sure all of their folds line up
Juvenile •
Children age 3-10
•
Testing them in a school environment. Usually on the later age of this group. Tthey go to the nurse and the nurse tells them to bend over touch their toes. She’s going to run her hand down their back to look for any type of scoliosis.
Adolescent •
Older than 10 years
•
Most common type
•
Occurs during the growth spurt of early adolescents
•
Most noticeable during this time
•
Adolescents are very egocentric appearance . They are thinking about opposite sex and their sexuality. If their clothes aren’t fitting correctly because their shoulders or their shoulder blades or their hips are not lining up then they’re gonna start complain about that and see a doctor to see what is causing the issue
Treatment based on: •
Magnitude
•
Location
•
Type of curve
•
Age and skeletal maturity of child/adolescent
•
Underlying and contributing disease process
MUSCULOSKELETAL OR ARTICULAR DYSFUNCTION •
Scoliosis Treatment •
•
Bracing •
Treats mild to moderate curvatures
•
Not curative but help maintain alignment until we can get to actually do surgery
•
Exercise is used in conjunction
•
Maintain and increase the strength of the spine and abdominal muscles
•
Maintain that alignment until they can do surgery. Something that the child is in for as many hours of the day as they possibly can, it’s to help maintain that alignment, increased strength of those muscle of the spine and abdomen.
Surgery •
Correction of severe curves
•
When we do surgery, this is done in the adolescent population because if even if they have one of the earlier types of scoliosis and we found this before their adolescent. Once they go to that adolescent growth spurt, it will get worse.
•
This surgery is a very severe surgery, it is very traumatic for the child and it does have a lot of risk factors involved with it and so what we do when we go in and do surgical correction is, they will take an MRI right before that patient goes into surgery. The patient will go into surgery, they’re laying down flat on their stomach. They’ll make an incision from the top of their neck all the way down their spinal column and open them up. They’ll put a rod on each side of their spinal cord (15 degree picture) and they will actually drill through the spinal process of your spine. The things that stick out are more bolts connecting those two metal rods together.
•
After that is done and they close them up, they’ll go and they’ll do another MRI so that we see before and we see after and then they’ll do one a couple days later as your body’s kind of attacking and making this thing stronger. They’ll do another one just to make sure that everything is still on the alignment and place the way that they wanted it to be. It’s a very traumatic surgery. You’re obviously dealing with the spinal cord and so there’s lots and lots of complications that can happen with this. This is not something that we want to be doing multiple times. We want to try to go in and do it once and then you’re good to go. Those metal rods, they’ll live with them in their back for the rest of their life and so you know there is a lot of teaching that we have to do for this child and family after they get out of surgery.
•
We usually wait when they turn adolescent since it is extensive. The only time we do it early is when the organs are damaged. The curve is so severe that they’re having issues with organ functioning. They are having respiratory issues. When we go into the scoliosis repair, it’s very important to talk to parents and the child about realistic expectations related to this. This is a very expensive surgery. We give them a PCA pump since they are an older child and they can manage that pump. But even with being able to manage the pump the pain is never gonna go away. But we need to repair this as we do an MRI to see what the curvature is, what everything looks like.
•
We will typically cut an incision from the top of their neck down the spinal column. They’ll go and they’ll put two rods on either side of their spinal column and then they’ll put con...
Similar Free PDFs
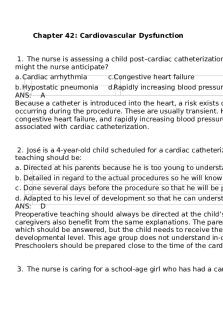
Ch42-Cardiovascular-Dysfunction
- 30 Pages

Sistema Articular
- 2 Pages

Soft Tissue Dysfunction
- 3 Pages

Cardiac Dysfunction Revised \'17
- 16 Pages

Papel articular - Apuntes 1.8
- 48 Pages

Semiologia Articular na Reumatologia
- 11 Pages

Mobilização articular
- 7 Pages

Musculoskeletal Exam
- 8 Pages

Woordenlijst OR verken 3
- 7 Pages

Musculoskeletal Disorders
- 40 Pages

Fisiología articular anatomia
- 11 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu




