Kinetics Exam Final Review April 27 PDF

| Title | Kinetics Exam Final Review April 27 |
|---|---|
| Author | Arian Hedayati Hedayati |
| Course | Pharmacokinetics/Biopharmaceutics |
| Institution | Massachusetts College of Pharmacy and Health Sciences |
| Pages | 41 |
| File Size | 1006.4 KB |
| File Type | |
| Total Downloads | 160 |
| Total Views | 901 |
Summary
Kinetics Exam 2 Study GuideLecture 5-6 Multi-compartment Models: IV Bolus Administration v Distinguish between one-compartment, multiple-compartment kinetics. v Introduces unique aspects of a multiple-compartment model v Calculate two -compartment model parameters by using the method of residuals. v...
Description
Kinetics Exam 2 Study Guide Lecture 5-6 Multi-compartment Models: IV Bolus Administration v Distinguish between one-compartment, multiple-compartment kinetics. v Introduces unique aspects of a multiple-compartment model v Calculate two-compartment model parameters by using the method of residuals. v Calculate clearance and alpha and beta half-lives of a two compartment model drug. v Discuss the impact of metabolic enzymes, transporters, and binding proteins Drug disposition following an IV bolus dose The Case for Extra Compartments • The presence of other compartments • Different Blood flow rates to tissues • Different permeability of drug into different tissues • Uptake of drug from plasma compartment by tissues • Binding of drug to tissues Some Tissue Groupings • Highly perfused tissues include: kidney, hepatic-portal system, brain and heart. • Poorly perfused tissues include adipose tissue, bone and hair Two Compartment Open Model • Central Compartment à k12 à Peripheral Compartment (k12 movement from compartment 1 to 2) • Central Compartment ß k21 ß Peripheral Compartment (k21 movement from compartment 2 to1) • k10 – elimination micro constant k20 – negligible elimination micro constant • When drug becomes bioavailable there is movement between compartments Phases of a Two Compartment Model • Distribution Phase and Elimination Phase – both are first order processes One Compartment Model • Before Dose: Large dose administered intravenously • After Dose: Instant thorough distribution throughout patient Two Compartment Model • Before Dose: Large dose administered intravenously • Right After Dose: Instant distribution only in some organs • Much Later After Dose: Later distribution throughout patient Two Compartment Model: Phases 1. Dose to be administered: no drug in either central (plasma) compartment or peripheral compartment 2. Instant distribution in first compartment only: drug in central compartment 3. Distribution Phase: net movement from central compartment to peripheral compartment - As soon as drug appears in peripheral it will also start to move back to central 4. Distributive Equilibrium: rate of drug in is equal to rate of drug out 5. Elimination Phase: drug is mostly in central compartment Phases of a Two-Compartment Model: Distributive Phase • Distributive Phase: drug level in plasma declines and drug level in periphery rises, but net transfer from the central to the peripheral compartment • Equilibrium: rate of drug entry into tissue equals the rate of exit • Elimination (Beta) Phase: drug levels in both compartments decrease in parallel t - Rate of decrease slower than in distributive phase - Mimics a reversion to a one-compartment model Rate and Hybrid Constants • Distribution Phase - ɑ, alpha; Ae-ɑt • Elimination Phase – β, beta; Be-βt • Cp = Ae-ɑt + Be-βt • Slope of Distribution Phase is always greater/steeper than slope of Elimination Phase (alpha > beta) Two Compartment Open Model: Some Important Equations • a + b = k12 + k21 + k • ab = k21k
• The intercepts A and B are constants but have no physiological significance • A = D0(a – k21) / Vp (a – b) • B = D0(k21 – b) / Vp (a – b) • Where Vp is volume of the central compartment Example A given drug used to treat depression follows first order (i.e. linear) 2-compartment pharmacokinetics. Values for a number of parameters for this drug have been documented. These numbers represent the micro constants for this drug. In order to calculate the drug concentration after a single IV bolus dose these parameters need to be converted into values for the macro constants. The k and Vp for this drug in this patient are 0.223 hr-1 and 40.2 L, respectively. The k12 and k21 values this drug are 1.53 and 0.96 hr-1 , respectively. Calculate the plasma concentration of this drug 4 hours after a 25 mg, IV Bolus dose.
Method of Residuals (aka “Feathering”) • The distribution phase is more rapid than the elimination phase i.e. a > b • Thus as Ae-at approaches zero, Be-bt will still have a value so the last equation becomes: Cp = Be-bt • So, logCp = -bt/2.3 + logB • When time is a large number (Ae-at = 0) so all of the Distribution is complete and we are only looking at elimination • b may be obtained from the slope of a semi-log plot of Plasma level against Time • Also by extrapolating the beta phase line on the semilog plot, B can be obtained (point at which residual line meets vertical axis) • A line representing the distribution phase is obtained by subtracting points (Cp ’) on the extrapolated beta line from the corresponding original observed data points (Cp ). • a is obtained from the slope of the Cp – Cp ’ against time plot Example A patient is given a 500 mg dose by intravenous injection and the following plasma concentrations result: Plasma Concentration (mg/L) Time after Dose (hours) 72.0 0.25 46.0 0.5 33.0 0.75 26.3 1.0 20.0 1.5 16.6 2.0 12.2 3.0 9.9 4.0 5.0 6.0 2.7 8.0 0.82 12.0
Two Compartment Open Model: Important Equations • k = ab (A+B) / Ab + Ba • k12 = AB (b – a)2 / (A + B) (Ab + Ba) • k21 = Ab + Ba / A + B Example A given drug follows first order (i.e. linear) two compartment pharmacokinetics. A 5 mg dose was administered by IV bolus and a number of blood samples were collected and analyzed for drug plasma concentration. After a successful analysis using the Method of Residuals values of A, B, a and b were determined to be 4.47 mg/L, 3.99 mg/L, 3.84 hr-1 and 0.9 hr-1 , respectively. Calculate k, k12 and k21 for this drug.
Apparent Volumes of Distribution: The Central Compartment Volume of the central compartment Vp (or Vi , the initial volume of distribution) is usually > 3 L (the average adult’s plasma fluid volume) i.e. distribution occurs outside the vascular pool • At time zero Cp0 = A + B • So Vp = D0 / (A + B) • The Vi is greater than the Vp Apparent Volumes of Distribution: Steady State • Dt = total amount of drug in tissues • Dp = total in the central compartment • The apparent volume of drug at steady state is given by the total amount of drug in the body divided by the plasma concentration at steady state: (VD)SS = Vp + (k12 / k21) Vp Apparent Volumes of Distribution: Extrapolated Obtained from the beta phase intercept of the plasma level-time curve • (VD)exp = D0 / B or… • (VD)exp = Vp (a – b / k21 – b) Apparent Volumes of Distribution: By Area • VDβ = clearance / b • VDβ = kVp / b Example A drug follows first order (i.e. linear) two compartment pharmacokinetics. A dose of 5 mg was given by IV bolus and a number of blood samples were collected and analyzed for drug plasma concentration. After a successful analysis using the Method of Residuals values of A, B, a and b were determined to be 4.47 mg/L, 3.99 mg/L, 3.84 hr-1 and 0.9 hr-1 , respectively. Calculate Vp , (VD )b and (VD )ss for this drug.
Apparent Volumes of Distribution: By Area • The expected decline in b in case of renal impairment could be masked if there is rapid redistribution between the plasma and the tissue. A change in k could account for the change in (VD )b Apparent Volumes of Distribution: Significance • (VD )exp > (VD )ss » (VD )b > Vp • (VD )b is more affected by the dynamics of the elimination phase whereas (VD )ss is a more accurate reflection of the general distribution of the drug. • For the purpose of modeling, assumed to be independent of clearance and other parameters • In reality factors such as drug binding, metabolism and uptake affect more than one parameter, rendering them not truly independent e.g. volume of distribution is not truly independent of clearance as depicted in models. Apparent Volumes of Distribution: Peripheral Compartment • The apparent volume of the tissue compartment: Vt = Vpk12 / k21 • Is an estimate of average drug build-up in body tissues (recall drug concentration will vary from tissue to tissue, or even between tissue samples) • Amount of drug in tissue may (Dt ) be more relevant to pharmacodynamics activity than the amount in the plasma • Dt = (k12Dp0 / (a – b)) (e-bt – e-at) • (See Example in notes) IV Bolus Two Compartment Model: Clearance • Model dependent method: Cl = (VD)βb IV Bolus Two Compartment Model: Elimination Rate Constant • k has to do with drug elimination from the central compartment • b has to do with drug elimination after the distribution is almost done i.e. the beta phase, and is affected both by the movement of the drug in to and out of the tissue compartment • b is therefore a hybrid constant • b Tissue Compartment > Deep Tissue Compartment • Central Compartment à k13 à Deep Tissue Compartment • Central Compartment ß k31 ß Deep Tissue Compartment Three Compartment Open Model: Equations • Cp = Ae-ɑt + Be-βt + Ce-ct • Vp = D0 / A+B+C Factors Determining the Number of Compartments • Assay sensitivity i.e. ability to detect low concentrations • Number of samples collected i.e. inappropriate sampling intervals • Route of administration • Rate of drug absorption • Total time for blood sampling Clicker questions 1. In a two compartment model at distributive equilibrium, rate of drug distribution from central to peripheral is equal – True 2. In a two compartment model at distributive equilibrium the concentration of drug in the central compartment is equal to the concentration of drug in the peripheral compartment – False
Lecture 7-8 Intravenous Infusion v Distinguish between an IV bolus dose and an IV infusion. v Discuss the concept of steady state within the context of iv infusions. v Calculate pharmacokinetic parameters from clinical data. v Calculate loading doses to be used with an intravenous infusion. v Describe the purpose of a loading dose. v Discuss IV infusions within the context of a two compartment model drug’s pharmacokinetics Drugs Following a One-Compartment Model • Infusion is typically a zero-order process - because rate is constant • For most drugs, elimination is first order – rate is not constant but depends on drug availability at a given time • On a Plasma Level vs. Time plot: - Increase concentration = Increase in elimination rate - Infusion rate > Elimination Rate – causes a rise in plasma concentration - Infusion rate = Elimination Rate – reached steady state - Stop infusing the drug and the plasma level drops steeply • The rate of change of the amount of drug in the body o dDB/dt = R - kDB • where R= the infusion rate; DB = amount of the drug in the body • Since DB= CpVD, following integration, the equation becomes o Cp= R/VDk(1-e-kt) • At infinite time, t= infinity and (1-e-kt) ≈1 o Cp= R/VDk • This represents the steady state of plateau phase, i.e. the plasma level at steady state o CSS= R/Cl o CSS= R/VDk o High R (infusion rate) value = increase in steady state concentration Example A desired steady state plasma level of theophylline maybe 15 mg/L. The average half-life of theophylline is about 4 hr. and the apparent volume of distribution is about 25 liters. What infusion rate is necessary?
Drugs Following a One-Compartment Model: The Steady State II • Equation may also be arrived at using the fundamental fact that at steady state, the ratein=rateout • i.e. Css is directly related to R and inversely related to the clearance (Cl) and the apparent volume of distribution (VD) Drugs Following a One-Compartment Model: The Steady State III • It takes an infinite amount of time to reach the true steady state i.e. the graph is asymptotic • The number of half-lives required to reach 90%, 95%, and 99% of steady state are 3.32, 4.32, and 6.65 respectively - 3.32 x t1/2 = 90% SS; 4.32 x t1/2 = 95% SS; 6.65 x t1/2 = 99% SS • NB: An increase in the infusion rate will increase the Css but will have no effect on the time needed to get there • t depends on K and t1/2
Drugs Following a One- Compartment Model: Calculating Patient t1/2 • k=-2.3/t log (CSS-CP/CSS) - estimate k • Thus, when given the approximate CSS and the Cp at a time t, k can be determined • Subsequently, the half-life can be determined from o t1/2 = 0.693/k (1st order processes) Example 1 An antibiotic has an elimination half-life of 3-6 hours in the general population. A patient was given an IV infusion of an antibiotic at an infusion rate of 15 mg/hr. Blood samples were taken at 8 and at 24 hours and plasma drug concentrations were 5.5 and 6.5 mg/L, respectively. Estimate the elimination half-life of the drug in this patient.
Example 2 If the desired therapeutic plasma concentration is 8 mg/L for the above patient (Example 1), what is a suitable infusion rate for the patient?
Drugs Following a One-Compartment Model: Simultaneous IV Loading Dose and IV Infusion • The total Cp at time t after the initiation of infusion: o Cp = C1 + C2 o Cp=R/VDK+ (DL/VDe-kt – R/VDK e-kt) Drugs Following a One-Compartments Model: Simultaneous IV Loading Dose and IV Infusion II • If loading dose is the amount of drug in the body at steady state, then: o DL = R / K • NB: If, DL ≠ R/K then steady state does not occur instantly - It will be at a higher or lower concentration than the steady state Drugs Following a One-Compartment Model: Clearance • Since k = Cl/VD : CP = R/Cl (1-e-(Cl/VD)tD)t) • The time needed to reach steady state is inversely related to clearance, given a constant apparent volume of distribution • This is important in patients with different renal functions and therefore different Clearances • NB: Cp=R/VDK(1-e-kb)e-k(t-b) – concentration when infusion has stopped • Where b= infusion time, t= total time, t-b = time after infusion has stopped • (See Example in Notes) Drugs Following a Two-Compartment Model: • This is the case for many drugs administered by IV infusion • Requires distribution and equilibrium before CSS is attained • At Css, drug levels in the tissue compartment remains the same • Using the hybrid constants, a, and b: o Cp= R/VPK[1-(k-b/a-b)e-at- (a-k/a-b)e-bt] • At t=infinity, Cp=Css this equation becomes: o Css=R/VPK • R=CssVpK
Drugs Following a Two-Compartment Model: Simultaneously IV loading Dose and IV Infusion • Drug distributes slowly into tissue compartment • It is not possible, using a zero-order infusion process, to attain a stable steady state instantaneously in a two-compartment model (loading dose is either slightly higher or slightly lower because you need to wait for distribution) - We need to allow for time to pass for distribution of drug Drugs Following a Two-Compartment Model: Apparent Volume of Distribution • The amount of drug in the body at steady state= Dp+Dt • (VD)SS= (Dp+Dt)/Cp • Where Dp is the total amount of the drug in the central compartment and Dt is the amount of the drug in the tissue compartment • At steady state: Ratein = Rateout • And o Dt= k12CpVp/k21 o (VD)SS= VP + (k12/k21)Vp • NB: (VD)SS depends on the transfer constants which depends on the drugs physical properties (such as the partion coefficient) Drugs Following a Two Compartment Model: Apparent Volume of Distribution II • (VD)ss is not affected by changes in the elimination rate of the drug • (VD)B, on the other hand is dependent on the elimination rate of the drug • (VD)B=D0/b[AUC]0infinity Clicker Questions 1. In a zero order IV infusion administration, an increase in infusion rate will increase the time needed to get to the steady state concentration (CSS) – False, this just increases the steady state concentration
Lecture 9-10 Drug Elimination and Clearance v Discuss the main routes of drug elimination v Examine Henderson Hasselbalch Equations within the context of renal drug elimination v Distinguish between clearance and renal clearance. v Discuss organ drug clearance in terms of blood flow and extraction. v Calculate clearance using different methods. Drug Elimination: Introduction • Drug excretion has to do with removal of unchanged drug (typically via the kidney but also sometimes via the lungs, breast milk, sweat etc….) • Drug biotransformation has to do with the enzymatic modification of the drug (facilitating its excretion and/ or altering its pharmacodynamic potential). Enzymes are usually hepatic but may be found in other tissues. • Drug Elimination = Drug excretion + biotransformation • Unlike clearance, elimination is not invariant for first order processes. Drug Elimination: The Kidney and Blood Supply • Receives 20 – 25% of cardiac output • Renal Blood Flow (RBF) = volume of blood flowing through kidney blood vessels per unit time • Renal plasma flow (RPF) = RBF – volume of red blood cells present - RPF = RBF (1 – Hematocrit) • For the average adult: • Hematocrit (Hct) » 45%; Glomerular filtration rate (GFR) » 125 mL/min • Filtration Fraction = GFR / RPF Drug Elimination: The Kidney and Urine Formation • Kidney regulates fluid volume as well as the levels of various solutes and electrolytes (Na+, K+) • GFR is controlled by hydrostatic pressure differences in the glomerulus. Kidney arterial pressure ~ 100 mmHg; drops to ½ its value in the glomerulus. • Average daily urine volume ~ 1- 1.5 L Drug Elimination: The Kidney and Drug Excretion • Renal drug excretion is a composite of glomerular filtration, active tubular secretion, and tubular reabsorption • Most small molecules (MW < 500) undergo glomerular filtration (no energy) • Proteins and protein-bound drugs do not undergo glomerular filtration • The GFR of a drug correlates well with the free levels of the drug in the blood • Inulin and creatinine are neither actively secreted nor reabsorbed; consequently, their clearances are ~ the GFR (125 – 130 mL/min). They used in the determination of the GFR. • • • • • • • • •
Active tubular secretion is an active transport process (requires energy input, is carrier mediated, the transported item is transported against its concentration gradient) Is dependent on renal blood flow Iodopyracet and p-amino-hippuric acid are both glomerulus-filtered and secreted by tubule cells; they are used to measure active tubular secretion; their clearances are a measure of the effective renal plasma flow (ERPF) The carrier system is saturable and can be the subject of competition by drugs of like structure There is a carrier system for weak acids, and one for weak bases Drugs bound to plasma proteins dissociate rapidly as they are secreted by the kidneys; consequently the elimination half-life of a drug excreted largely by secretion is unaffected by protein binding Tubular reabsorption can either be active or passive Un-dissociated (unionized) drugs are more lipid soluble and more capable of penetrating cell membranes; they are thus more easily reabsorbed - Ionized drugs stays within nephron and is then voided The extent of dissociation is governed by the Henderson-Hasselbalch equation i.e. it depends on the urine pH and the pKa of the drug
Drug Elimination: The Kidney and Drug Excretion • The Henderson-Hasselbalch equation for weak acids: pH = pKa + log [ionized] / [unionized] • Fraction of ionized drug = 10pH-pKa / 1 + 10pH-pKa • The distribution of a weak acid between urine (U) and plasma (P):
•
U/P = (1+10pHurine – pKa) / (1 + 10pHplasma – pKa)
• The Henderson-Hasselbalch equation for weak bases: pH = pKa + log [unionized] / [ionized] • The distribution of a weak base between urine (U) and plasma (P): • U/P = (1+10pKa – pHurine) / (1 + 10pKa – pHplasma) Example Phenobarbital is a weak acid with pka of 7.2. (i) Calculate the percent ionized in blood (pH 7.4). (ii) Calculate the percent ionized in urine (pH 6.4).
Example Itraconazole is a weak base with a pKa of 3.8. (i) Calculate the percent ionized in blood (pH 7.4). (ii) Calculate the percent ionized in stomach (pH 1.8).
Example A 39 year old woman is admitted to an emergency room following a phenobarbital overdose. Her urine pH is 5.8 at the time of admission. She is given 9g of sodium bicarbonate IV over 24 hours to alkalinize the urine. If her urine pH afterwards is 8, by how much is the resorption of the phenobarbital reduced? (about 30% phenobarbital is eliminated by kidneys and phenobarbital pKa = 7.24; assume blood pH is 7.4) (Phenobarbital is a weak acid)
Drug Clearance • Alternatively, ClT = elimination rate / plasma concentration (Cp) • Elimination rate = CpClT • Since amount of drug eliminated: DE = CpVD • ClT = kCpVD / Cp = kVD, so ClT = kVD • Total body clearance = renal cleara...
Similar Free PDFs

Kinetics Exam Final Review April 27
- 41 Pages

COM200 UILG TMA 27 April Final
- 41 Pages

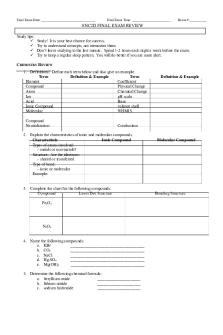
Chem Final Exam Review
- 12 Pages

Final Exam - Review notes
- 92 Pages

Bio Final Exam Review
- 2 Pages
Final EXAM Review booklet
- 5 Pages

CHEM303 final exam review
- 4 Pages

Psychology Final Exam - Review
- 13 Pages

Jarvis Final Exam Review
- 12 Pages

Final exam review
- 96 Pages

Final Exam Review
- 48 Pages

Marketing Final Exam Review
- 15 Pages

Final exam review
- 8 Pages

Astronomy Final Exam Review
- 2 Pages
Popular Institutions
- Tinajero National High School - Annex
- Politeknik Caltex Riau
- Yokohama City University
- SGT University
- University of Al-Qadisiyah
- Divine Word College of Vigan
- Techniek College Rotterdam
- Universidade de Santiago
- Universiti Teknologi MARA Cawangan Johor Kampus Pasir Gudang
- Poltekkes Kemenkes Yogyakarta
- Baguio City National High School
- Colegio san marcos
- preparatoria uno
- Centro de Bachillerato Tecnológico Industrial y de Servicios No. 107
- Dalian Maritime University
- Quang Trung Secondary School
- Colegio Tecnológico en Informática
- Corporación Regional de Educación Superior
- Grupo CEDVA
- Dar Al Uloom University
- Centro de Estudios Preuniversitarios de la Universidad Nacional de Ingeniería
- 上智大学
- Aakash International School, Nuna Majara
- San Felipe Neri Catholic School
- Kang Chiao International School - New Taipei City
- Misamis Occidental National High School
- Institución Educativa Escuela Normal Juan Ladrilleros
- Kolehiyo ng Pantukan
- Batanes State College
- Instituto Continental
- Sekolah Menengah Kejuruan Kesehatan Kaltara (Tarakan)
- Colegio de La Inmaculada Concepcion - Cebu

